News
Diabetes monitoring technology an ‘empowering’ patient tool
New data has shown the positive impact of flash glucose monitoring for people with type 2 diabetes.
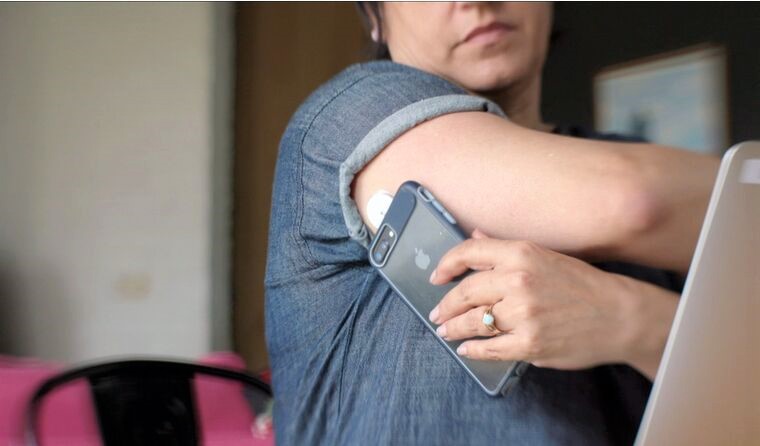 Similar to a continuous glucose monitor, flash technology features a sensor that is scanned with a smartphone or reader to obtain a glucose reading.
Similar to a continuous glucose monitor, flash technology features a sensor that is scanned with a smartphone or reader to obtain a glucose reading.
Close to one million adults in Australia have type 2 diabetes.
According to a new report released by the Australian Institute of Health and Welfare, more than 16,600 people in 2019 alone started using insulin to manage their condition for the first time.
Continuous glucose monitors (CGM) are among a suite of technology that is emerging in diabetes management, and new research has shown the benefits for improving glycaemic control among people with type 2 diabetes.
Preliminary data from an observational study of 774 people with type 2 diabetes on insulin therapy using a flash glucose monitoring system saw a reduction in HbA1c from baseline by -0.6% after six months, and by -0.5% after 12 months.
The technology was also shown to be beneficial for people on non-insulin therapy, with a reduction in HbA1c by -0.9% after six months and -0.7% after 12 months.
Lead author Dr Eden Miller, a US-based GP with a special interest in diabetes, was surprised by the results.
‘The part that I was surprised about is the cohort that was not on insulin had a better improvement in their HbA1c than the cohort on insulin,’ she said.
‘I didn’t expect the magnitude. I expected similar – actually, [I] probably expected the reverse.’
Further research by Dr Miller of 7167 people with type 2 diabetes using the technology also noted a 30% reduction in acute diabetes events, and a 13% drop in the rate of hospitalisations.
Dr Gary Deed, Chair of the RACGP Specific Interests Diabetes network, told newsGP that while it is early days, that the findings are a step in the right direction to support further clinical use of CGMs and flash technology.
‘I don’t want to over read the articles as being conclusive proof,’ he said.
‘But it’s adding to the emerging evidence that what we experience in clinical practice is being supported by increasing quality evidence.’
The flash glucose monitoring system allows people with diabetes to check their level via a small sensor placed on the back of the arm. A filament penetrates the skin into interstitial fluid, and a glucose reading is gathered by hovering a smartphone or a reading device over the sensor.
The data is then gathered in an app and can be shared with the person’s GP via a secure cloud-based platform.

Dr Gary Deed says glucose monitoring technology can be an empowering tool for particular patient cohorts.
Dr Deed, who has a number of patients using the technology, says it is a more patient-friendly way to test glucose levels.
‘We are encouraging people to do self-monitoring of glucose and that process, up until changes in technology, would involve multiple finger-prick testing during a day and maybe more often,’ he said.
‘This sort of technology, particularly the flash glucose technology, reduces the need for multiple daily glucose finger pricking. There may still be a need for it, but in the majority of cases it allows the patient to have almost instant ability to assess the glucose in a more discreet, but also less painful way.’
There is a delay of up to 20 minutes behind the blood glucose level. The technology includes trending arrows that can tell the person whether their glucose is rising, falling or stable at that particular level.
‘We try to have what we call “time in range”; that is a glucose level where we know that’s associated with safety for the patient and associated with health outcomes. The range is set between 3.9 and 10 millimoles per litre,’ Dr Deed said.
‘But say my glucose was at four when I tested on my flash monitor and the arrow was pointing down, it would also explain to me that maybe I need to retest in a shorter interval because I might be going into what we call the hypoglycaemic range.
‘The same applies with an elevated glucose. It allows you to connect a number to action, which associated with education is a much more patient-focused self-management support technique.’
Dr Deed says this insight helps to empower patients by giving them greater understanding of what their glucose is doing, and the actions they can take.
‘Technology that allows you to understand the variations in how you live, how you exercise, how you eat, and its effects on glucose is very empowering,’ he said.
‘It’s connecting people back to their illness not necessarily negatively, but more in an empowering way to say “I can now do something if my glucose is low or high” rather than feeling I have to wait three months to see the doctor to tell me what to do.’
Yet when it comes to glucose monitoring devices, equitable access remains the biggest barrier.
Diabetes in Australia is almost twice as prevalent among those living in the lowest socioeconomic areas.
On 1 March, the Federal Government expanded subsidised access to a flash glucose monitoring device for certain cohorts with type 1 diabetes. But for people with type 2 diabetes, however, there is little support.
‘This is one of my biggest bugbears around technology is issues of equity, and also not increasing in equity,’ Dr Deed said.
‘When it comes to type 2 diabetes, there’s currently not supported access through the Government scheme. However, private health insurance may support those that wish to have access to it.
‘I think that inequity may improve in time once technology costs, etcetera, are reduced.’
GPs have an important role to play in advocating for patients, Dr Deed says, and to do so means staying abreast of advances in technology.
‘It actually challenges general practice to … really keep up to date with education around this because the last thing you want is a patient who comes in with this technology and, in fact, you yourself don’t even understand or haven’t come across what it means,’ he said.
‘It’s a real call to action.’
GPs can find out more about CGMs and the patient eligibility criteria for subsidised access on the National Diabetes Services Scheme website.
Log in below to join the conversation.
diabetes flash glucose monitoring type 2 diabetes
newsGP weekly poll
What is your chief concern with role substitution?