News
Growing number of Australians reject COVID vaccination
Vaccine hesitancy has soared since recommendations shifted from AstraZeneca to Pfizer for under-50s.
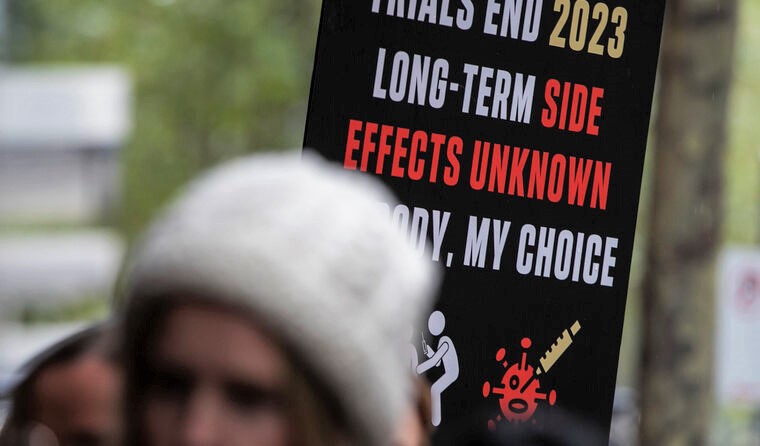 One in six Australians say they will never get vaccinated against COVID-19, an increase from March. (Image: AAP)
One in six Australians say they will never get vaccinated against COVID-19, an increase from March. (Image: AAP)
There’s no denying it – nine weeks into Australia’s vaccine rollout, and confidence is waning, according to the latest Essential Report.
The survey completed online by 1090 people between 21–26 April, found just 43% of Australians think the rollout is being done efficiently, down from 68% in March; 63% think it is being done safely, down from 73%; and just over half (52%) are confident the vaccines will be effective at stopping COVID-19.
The slow rollout and changes to the roadmap also appear to have given rise to vaccine hesitancy, with one in six people (16%) saying they will never get vaccinated against COVID-19, up from 12% last month, while 42% said they will get vaccinated, but not right away.
The proportion of people who would be willing to get vaccinated as soon as possible, or are already vaccinated, also declined, down from 47% to 42%.
Men (49%) were the most likely to report a willingness to get vaccinated immediately, as were people over 55 (53%); however, that has dropped by 7% since last month.
The poll also showed that just 37% of people are willing to get either the AstraZeneca or Pfizer vaccines; 27% are only willing to receive Pfizer, 14% said they do not want either vaccine, and 19% said they are unsure.
The findings follow emerging concerns over the AstraZeneca vaccine and six reported cases of blood clots, which saw the Australian Technical Advisory Group on Immunisation (ATAGI) recommend Pfizer for those under 50.
While the Government has made clear that AstraZeneca is safe for those over 50, going so far as to bring forward their eligibility date, just 40% of people aged 50–69 said they are currently willing to get either vaccine.
The findings are in line with the experiences of some GPs who have reported patients failing to show up for their vaccine appointments, while the latest dose utilisation figures from the Federal Department of Health reveal a number of doses are going unused in fridges.
Associate Professor Holly Seale is a social scientist with UNSW Medicine’s School of Public Health and Deputy Chair for the Collaboration on Social Science and Immunisation.
She told newsGP while the survey is a relatively small sample, it is clear the national COVID vaccination campaign needs ‘a shake-up’.
‘If people aren’t turning up to a general practice, that presents a challenge – regardless of the type of mass media we have,’ Associate Professor Seale said.
‘We’ve got to be mindful that we’re in a very different phase now, and while a huge amount of people still listen to radio and watch television, it doesn’t talk to everybody. We need to think about other ways.’
Drawing on her insight from working to address vaccine hesitancy among culturally and linguistically diverse communities, she says there is a need to ‘decentralise’ communications by tapping into different networking spaces, such as workplaces, local gyms, mothers’ groups, and seniors’ clubs with a focus on all age groups, regardless of current eligibility.
‘For example, organisations have staff occupational health and safety programs already embedded and for years have been offering flu vaccination,’ Associate Professor Seale said.
‘Can we get GPs and primary care nurses to be partnering with these organisations to actually have a chance to go in and do a half-an-hour presentation or Q&A session?
‘So many times, people have said to me, “It’s so useful to have that opportunity to just ask those questions”. We know that if you get to the person in advance and get them thinking and writing down any questions, the quality of conversation is much better when the person reaches the GP consultation room – that’s been found in the past.’
Meanwhile, Associate Professor Seale says general practices can also take an opportunistic approach to educating patients about the coronavirus vaccines.
‘I went to have my flu vaccine the other day, and while I’m yet to be recommended a COVID vaccine in terms of eligibility, as I was sitting for 15 minutes post-vaccine, could that have been a time for me to be looking at some information? Or just to even have that chance to talk to someone and ask a question?’ she said.
‘This is what we may need to be doing.’
Authorities and vaccine experts have consistently maintained that transparency around the vaccine rollout is key to ensuring confidence, yet that is contrary to the report’s findings.
While Associate Professor Seale agrees that openness is important, she says the challenge is ensuring emerging information is adapted for the intended audience.
‘That’s what I’m a little bit concerned about at the moment; there’s a lot of resources on government websites, but these terms around blood clotting are very technical,’ she said.
‘We actually need to make sure that we are breaking them down in a way that will make it meaningful to people. That’s not just about translating, it’s about being conscious of people’s health literacy needs too. So maybe getting some more visuals into materials to try and support that.’
While a three-day lockdown was imposed in Western Australia recently, Associate Professor Seale says the relatively low community transmission may mean the prospect of lockdowns is not enough to encourage vaccine uptake.
‘How are people considering the risk of COVID? Is it based on what we are currently experiencing – back to having no lockdowns for most of Australia and very little in the way of any other measures currently in place?’ she said. ‘This is what we now need to start teasing out more.
‘It may be other things that we need to now start focusing on … that will start to promote and motivate people, such as the chance to travel more freely for example.’
While the survey has raised concerns, Associate Professor Seale says there is some variation in the findings that signals hope.
‘There’s a whole combination of things happening at the moment and the confidence will vary over the time of the program – that’s nothing new. Think about things like the MMR vaccine and autism issues back in the 90s, confidence changes,’ she said.
‘While this rollout continues and matures, it’s going to support uptake eventually. But in the meantime, we are going to have these ebbs and flows in people’s acceptance of the particular vaccines.
‘What we want to work on along the way is ensuring good confidence in the program … because if we put this all in a negative lens, then we’re not going to get anywhere.
‘So we need to learn from this – and learn quite quickly.’
Log in below to join the conversation.
AstraZeneca Pfizer vaccine hesitancy vaccine rollout
newsGP weekly poll
Is it becoming more difficult to access specialist psychiatric support for patients with complex mental presentations?