News
Anxiety and depression medication rates spike amid ongoing uncertainty
Experts have long predicted the coronavirus – and the lockdowns needed to curtail it – will lead to a long tail of mental health impacts.
 Experts have cautioned that prescribing mental health medication for pandemic-linked issues should not be the default option.
Experts have cautioned that prescribing mental health medication for pandemic-linked issues should not be the default option.
Now those impacts can be quantified, with prescription rates of anxiety and depression medication rising by substantially in recent months, according to aggregated Outcome Health data from more than 1000 Australian general practices.
Anti-anxiety drugs in particular have soared by up to 31%, suggesting uncertainties over health and financial impacts are taking their toll, while antidepressant prescriptions have also risen steadily, up by double-figure percentages (13–22%) over last year for each of the eight weeks ending 6 June.
The trend has led experts to caution that prescribing mental health medication for pandemic-linked issues should not be the default option, with non-pharmacological interventions like exercise or relaxation techniques often tried first.
‘We can see that whilst there is a steady increase in the use of antidepressants, there has been a marked recent increase in anxiolytic prescribing, most notably for diazepam,’ the Outcome Health paper on mental health impacts states.
‘The trend [for mental health medication] is rising, and we expect that it will continue to do so for some time as the consequences of isolation, fear around COVID-19, social circumstance and the economic impacts persist in the coming months.
‘[This] is a measure of those who are seeking treatment, and it is significant. We have seen an increase in the use of pharmacotherapy, and a significant shift to the use of telehealth in supporting the care of mental health patients.’
While rates of mental health consultations and prescriptions for mental health drugs fell during the initial lockdown, new mental health diagnoses have increased since mid-April, with people with existing mental health conditions seeking more care from their GP.
Outcome Health research director Associate Professor Chris Pearce told newsGP the paper shows there is ‘proportionately more anxiety than depression’ occurring.
‘That makes sense given what’s happening,’ he said.
‘We predicted in an earlier paper that there would be a slow increase in mental health issues in this phase, and that’s happening as the longer-term impacts of lockdown and coronavirus come into view.’
An earlier Outcome Health paper on medication trends claims that the ‘rigours of lockdown have increased the anxiety levels in the community’.
Antipsychotic medication rates have also shot up, though Associate Professor Pearce attributes that to the fact GPs are increasingly taking up this role rather than hospitals.
‘People have always sought mental health care from GPs. But over the last few years, they have become integrated and recognised as part of the system,’ he said.
Mental health has become the single largest issue for which patients seek care from their GP, according to the RACGP’s 2018 Health of the Nation report.
Associate Professor Pearce believes practice nurses can play a key role in combatting the spike in mental health issues by undertaking check-ins by phone – if they were able to access telehealth MBS items.
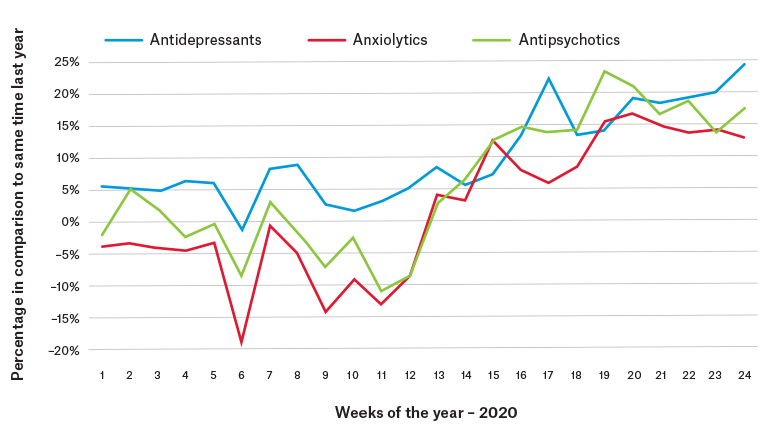 Rates of antidepressant, anxiolytic and antipsychotic use in 2020. (Source: Outcome Health: Mental Health Impacts of COVID-19)
Rates of antidepressant, anxiolytic and antipsychotic use in 2020. (Source: Outcome Health: Mental Health Impacts of COVID-19)
GP and Melbourne University senior lecturer Dr Caroline Johnson told newsGP the news is concerning, but not surprising.
‘The optimistic view is that data showing increased help-seeking by patients confirms the success of mental health education and stigma reduction and people know it is important to seek help,’ she said.
‘The pessimistic view is that these figures represent the tip of the iceberg of people experiencing distress, with widespread unmet need that may or may not subside as our communities learn to adjust to the “new normal” of a prolonged pandemic.
‘I am concerned that just as we have seen increases in alcohol consumption during the pandemic, people may be turning to short-term pharmacological solutions, like benzodiazepines, to reduce distress quickly. Unfortunately, this may create more problems for patients – and their doctors – in the long-run.
‘As a GP, I know how difficult and time-consuming these conversations can be. Encouraging someone who is very anxious in the context of the pandemic to see a psychologist or sign up for an [emergency mental health] program sounds sensible, but if the patient is not sleeping, not thinking clearly and wants something to cope quickly, medications will inevitably be an option that gets raised.
‘Telling a patient that an SSRI might help for anxiety but might take a few weeks to work and then you might have to stay on them for 6–12 months or longer is not always appealing to a patient who frames their distress very much in the immediate context of a pandemic.
‘So what does this mean for GPs? Well, we need to be really careful not to reach for the prescription pad too readily, and if we do decide to prescribe psychotropic medication then try our best to match the treatment to the diagnosis.
‘There is a lot of sub-threshold depression and anxiety in the community at the moment and for these patients the evidence doesn’t support prescribing medication.’
Dr Johnson believes GPs should instead consider prescriptions for other, non-pharmacological strategies like exercise, activity-scheduling, relaxation techniques and structured problem solving, with many online courses readily available.
These techniques, she believes, have become easier for GPs to recommend and encourage through the use of regular telehealth consultations to check in and keep patients on track.
‘Increased help-seeking is good, but it may be contributing to the age-old problem in general practice of how to quickly respond to an emotionally distressed patient when working in a high-time-pressure fee-for-service environment,’ Dr Johnson said.
‘Telehealth has made this easier, and the advice can be broken up into steps delivered over three or four standard appointments, which in part addresses the other long-term problem for GPs that spending too much time with a patient leads to negative impact on practice income.’
Log in below to join the conversation.
anxiety depression mental health pandemic
newsGP weekly poll
What is your chief concern with role substitution?