Feature
These GPs worked with Australia’s most vulnerable patients – until the compliance crackdown
The reward for the hard work these GPs put into treating body and mind? Unfair punishment, they claim.
 While only 341 GPs received the letter, it has generated outrage throughout general practice.
While only 341 GPs received the letter, it has generated outrage throughout general practice.
For two GPs from the US and the UK, Australia’s system of universal healthcare has been a boon.
It has given them the chance to provide holistic mind–body health advice and tackle patients with complex mental and physical issues – the challenging work they love to do.
Until now, at least.
As they tell newsGP, the recent Department of Health (DoH) crackdown on co-claiming mental and physical health Medicare Benefits Schedule (MBS) items has left them bruised.
One GP, Dr Susan Tyler-Freer, has left general practice entirely, while the other, a Sydney GP who wishes to remain anonymous, is considering his options.
Meanwhile, a patient concerned by the compliance campaign has told newsGP that her GP effectively saved her life by treating her mind and body while she experienced severe depression.
‘I can tell you, unequivocally, that once I finally got the nerve to get to my GP, it was critical that I be able to share my mental health issues at the same time as I was talking about the physical issues that eventuated from my mental health state,’ the patient told newsGP.
‘I can tell you without a doubt that I would be dead from suicide if I had not been treated holistically.
‘I am not being overly dramatic when I say that. It is a fact.
‘It is bad enough that people are slipping through the cracks these days due to waitlists. If they cannot speak their mind when they finally get to see someone, there is a missed opportunity to save a life.’
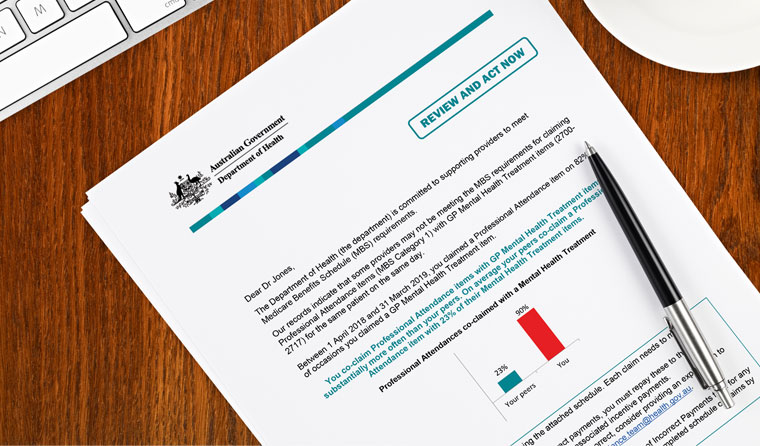
The now-infamous compliance letter targets over-claiming of mental health and physical health MBS items.
Though only received by 341 GPs, their general practice colleagues around Australia have been angered by what they perceive as a crackdown on holistic health – treating the whole person.
The DoH has defended the letter, with a spokesperson telling newsGP there is ‘absolutely no suggestion that it is not appropriate to treat mental and physical conditions in the same consultation’.
But many doctors feel the letter has created unnecessary fear and anxiety far beyond the actual number of recipients.
RACGP President Dr Harry Nespolon has called for an immediate end to the campaign, after the RACGP repeatedly expressed its concern over the growing trend of compliance by algorithm, where GPs who claim specific items or combinations of items more than their colleagues may be sent a warning letter.
The flaw in this thinking, the RACGP has argued, is that outliers can also be explained by specific patient cohorts. GPs with a special interest in palliative care, for example, are likely to prescribe more opioids than average, because their patients are dying and in pain.
And GPs like this Sydney doctor who choose to work with vulnerable and challenging cohorts may well co-claim more mental health items alongside physical health.
Despite widespread concerns, the compliance campaign has not been pulled.
Federal Health Minister Greg Hunt has instead asked the DoH to work with the RACGP and other key medical groups regarding their proposed improvements for greater clarity on claiming these items.
A DoH spokesperson told newsGP the department accepts that individual practitioners ‘may have a particular type of practice or patient cohort that leads to higher co-claiming of mental health items and professional attendance items than average’.
‘In this situation, doctors are advised that if they are satisfied that their practice is appropriate, no further action is required,’ the spokesperson said.
But the two GPs who have spoken out about their experience both have complex patient cohorts which, they argue, should have explained their claiming.
‘It broke my heart’
Up until last year, Dr Susan Tyler-Freer was doing precisely the type of medicine she wanted to offer people.
All of the patients at her general practice in the hinterland of Byron Bay had complex, challenging issues – PTSD, serious mental health issues, and addiction.
To unpick their issues took time. Almost all of her consultations were 45–60 minutes.
She also worked in palliative care, with 60–90-minute consultations the standard.
This was what Dr Tyler-Freer loved about medicine – dealing with the complexity and challenge of mind and body.
But then she received a phone call from a doctor employed by the DoH’s Professional Services Review (PSR). It was a forerunner of the compliance letter.
The doctor from the PSR wanted Dr Tyler-Freer to explain why she was co-claiming so many mental health items alongside professional consultation.
She talked about her patient cohort and the type of medicine she did.
The PSR doctor was sympathetic and far from cold-hearted, according to Dr Tyler-Freer. But it was made clear that the rules were the rules and her claiming was outside the normal range.
Patients had to intend on seeing her for one reason, and then disclose a second reason. They could not simply tell her about both mental and physical issues ahead of time.
What, she asked, should she tell her patients? Come back twice? What about those who had to carefully plan around their disability pension date?
The answers she heard did not help her concerns.
The PSR doctor told her she would have to be monitored for a year to ensure her mental–physical co-claiming shifted closer to her peers.
But improving the numbers meant Dr Tyler-Freer would have to move away from the type of complex medicine she loved.
Rather than do that, she quit general practice.
‘I was so disheartened after that phone call that I gave up practising. It broke my heart. I loathe this situation,’ she told newsGP.
‘I had people taking three buses with their carer to get to an appointment. I wasn’t going to get them to come to two. They were barely coping as it was.
‘We took the heartsink patients and we were seeing successes. With enough time and attention, you can get successes.
‘So this was the straw – without being able to do it that way, I couldn’t continue. I was not interested in doing things that were not meaningful or unlikely to be successful.
‘Having someone come in every fortnight for an hour with full attention to everything was making a difference to people. I was more than happy to work that way. I wanted to do proper slow care.’
Dr Tyler-Freer now works out of hospital and sees a handful of home-visit patients.
And Byron Bay’s hinterland has lost a good GP.
Dr Tyler-Freer said she is ‘pretty good’ at her work and would like to return, but the present atmosphere of anxiety would have to lift before she would consider risking returning to the work she loves.
The crackdown has made her doubt Australia’s healthcare system for the first time.
‘I really believe in Medicare,’ she said. ‘I come from a country [the US] without a coherent health system. You have a system [in Australia] where people are entitled to healthcare and that’s a good thing.
‘But having the system tell me I’d been doing the wrong thing and needed to be watched – I felt like I’d placed a lot of trust and faith in the system.
‘Now I feel like I can’t be part of it anymore.’

Having to go back through hundreds of previously billed items can create hours of work – and considerable anxiety – for GPs who received the letter.
‘I’m always going to be an outlier because my patients are outliers’
When a Sydney GP received a letter from the DoH last week, his heart sank.
Was it a complaint from a patient?
No. It was worse.
He had received a warning letter over his co-claiming of mental and physical health items.
The Sydney GP – who does not want to be named – told newsGP the letter is hugely unfair.
Why? Because he has spent his career treating patients in very difficult circumstances, ranging from people experiencing homelessness to those with drug and alcohol dependencies to people living with HIV.
He believes it is for that exact reason – the fact he spends serious time trying to loosen the complex knot of problems – that he appeared on the DoH’s statistical radar.
The Sydney GP feels he is being punished for doing a good job.
‘I’m always going to be an outlier because my patients are statistical outliers,’ he told newsGP. ‘I very rarely do a six-minute consult because that’s just not the nature of the patients I see. They’re not just here for a prescription or a blood pressure check.
‘I see the hard-to-reach, the vulnerable, I see the addicted patient who has tried to find help elsewhere and not been able to.
‘You feel like you’re able to do something good, and then you get a letter like this. I know I’m not fraudulent. I feel like I’m providing a service not many do.’
Three of the GP’s colleagues have also received the letter, and they all have similar patient cohorts.
‘It’s almost guaranteed that someone with a drug or alcohol dependency will have a physical comorbidity,’ the GP said.
‘People with HIV will often have mental health issues and will need STI screening and medication monitoring. People who are homeless often can’t afford to pay a gap and can be hard to reach. So when they come, you want to do as much opportunistic healthcare as you can.
‘Co-billing enables you to do that more comfortably.’
He said receiving the letter was ‘the last thing you ever want to see’.
‘This is worse than getting a complaint,’ he said. ‘You’ve got to go through all these consultations and pay back money – and you can’t even really see what it is that you’ve done wrong.’
Though his medical defence organisation has advised him to keep quiet and pay back any money owing, the GP is determined to speak out.
After all, it was for this reason that he left the UK’s beleaguered NHS service.
‘I got a very similar feeling in the NHS when I worked there, and I left the UK for this exact reason,’ he said. ‘You had the media vilifying GPs for being greedy, when in reality you were doing all this work for free. It was a thankless task, and you were doing it with no pay rises, just pay cuts.
‘All around me, GPs were burning out. That’s why I left to come here.
‘This letter smacks a bit of [the NHS approach].’
The letter has shaken him deeply.
‘Already my billing has changed. It’s triggering,’ he said. ‘Even if I know the claim is okay, I just can’t bring myself to do it.’
Immediately after opening the letter, the GP saw a patient who had booked a longer consultation. She wanted a skin check and to talk about her mental health care plan and her muscular pain.
But, affected by the letter, the GP did not claim the items to which he was entitled. Instead, he claimed a single item – effectively giving himself a major pay cut.
‘My anxiety has increased 100-fold in dealing with this group of patients,’ he said. ‘If I don’t regain my confidence, I’ll naturally shorten my appointments and just stick to one problem per appointment.
‘Why have they gone after these items? Why are they going after GPs who have a high rate of complex patients?’
Patients who are homeless often have chronic pain and challenges with addiction. There are almost always mental health issues, and sometimes complex mental health issues like schizophrenia or severe depression.
In his broader group of patients, he sees cellulitis, skin infections, rashes and asthma or COPD linked to smoking.
‘With any addiction, you’re at higher risk of all these things – and they go neglected until it’s a crisis,’ the GP said.
‘You get patients coming in with a raging dental abscess because they can’t afford to see a dentist. That small rash has become infected because they haven’t seen a GP.
‘They come to me when things are bad, and it just takes time to unpick.’
As a result of the letter, the GP will now have to review 900 items spanning 13 months.
‘It will take at least two full days. I haven’t started because I can’t face it,’ he said. ‘I’ve already paid tax on this and paid practice fees. Now I’ve got to give it back. It’s a real kick to the teeth.
‘I’ll be reading harrowing patient stories where I know I gave good service, and then pay the money back. These are patients bulk-billed who I’ve spent at least 30 minutes with.’
The GP he said he had been drawn to this kind of work because of the challenge.
‘In the addiction field, there’s a huge unmet need. That’s where mixed billing practices are really nice – you see the patients who can afford to pay and that frees up your time so you can give good service to the vulnerable who can’t afford to pay,’ he said.
‘When I do rehab work, these are people in recovery who want to make a change. It’s rewarding work.’
The GP said he felt bitter about the warning technique.
‘It’s working, isn’t it? They get money off me, I change my billing,’ he said. ‘Why shouldn’t they keep doing it? I hope once my confidence returns, my billing will return.
‘Why are they going after vulnerable patients and GP specialists when we earn so much less than any other doctor and don’t get the support of annual or sick leave that other specialists often do?
‘We’re being squeezed.’
The small silver lining to date has been a groundswell of support from his colleagues and from the profession more broadly. He also advises speaking to a medico-legal adviser, to get clear advice and support.
As the shock fades, anger is beginning to set in.
‘At the moment I’m shackled. I’m going to try to put my ego to one side, pay some money back and hope it’s done and dusted,’ he said.
‘But after that, I can start to get a bit angrier.’
Log in below to join the conversation.
compliance Department of Health Medicare Benefits Schedule
newsGP weekly poll
What is your chief concern with role substitution?