Background
Bunions are a common complaint, particularly among older female patients. They are characterised by progressive deformity at the metatarsophalangeal joint, resulting in a painful dorsomedial prominence. This may cause difficulties with shoe wear and contribute to falls in the elderly.
Objective
The aim of this article is to discuss the aetiology, non-operative and operative management of bunions, as well as indications for referral.
Discussion
Initial treatment of symptomatic bunions should be non-operative. Accommodative footwear is important. There is evidence supporting the use of nonsteroidal anti-inflammatory drugs, orthotics, splints/braces and toe spacers. However, these may not provide long-term relief, and referral to an orthopaedic surgeon is recommended if the patient has a painful prominence, has exhausted non-operative treatment and is a suitable operative candidate. Cosmesis alone is not an indication for operative management. Smoking is a relative contraindication to surgery, and cessation is recommended. In paediatric or adolescent patients (juvenile bunion), surgery should be delayed until skeletal maturity.
Bunions, also known as hallux valgus, are a common forefoot condition characterised by deformity at the great toe metatarsophalangeal joint (MTPJ). The great toe deviates laterally and the metatarsal deviates medially, resulting in a painful prominence at the dorsomedial aspect of the metatarsal head (Figure 1).
Australian patients seek general practitioner (GP) treatment for bunions at a rate of 4.2 per 10,000 encounters.1 Increased prevalence is seen in women and older patients. In the Australian population, 82.3% of patients who present to their GP with bunions as their chief complaint are female, and 80.5% of patients are aged ≥45 years.1 The overall prevalence in the adult population is 23%.2 Juvenile bunion (paediatric hallux valgus) can be defined by the presence of an open growth plate, and it is rare.3 The majority of patients are female, and half present before 10 years of age.3
Bunions are a common foot complaint, and patients may present to their GPs seeking advice or referral to an orthopaedic surgeon. The aim of this article is to review the non-operative management of bunions, as well as provide a brief overview of operative treatment and indications for referral.

Figure 1. Typical bunion deformity
Aetiology
Patients often present with medial forefoot pain and difficulties with shoe wear. Bilateral deformity is common.4 The most common source of pain is the dorsomedial eminence; however, patients may complain of pain under the lesser toe MTPJs (transfer metatarsalgia) due to the loss of effective weight-bearing through the first ray.4,5 Patients frequently have associated lesser toe deformities (such as hammer toes) and painful plantar keratosis.5 Severe deformity can lead to altered gait biomechanics and an increased risk of falls in elderly patients.6 The natural history of bunions is generally progression of deformity over time, rather than stable symptoms or improvement.
Despite many proposed causes, the exact aetiology of hallux valgus is unclear. Many patients have a positive family history for bunions, and there is likely a heritable component.4,7 While often implicated, a causative relationship between bunions and footwear, particularly high heels, has not been shown in the literature.8 Pes planus (flat foot) and generalised ligamentous laxity may contribute to juvenile bunions.3
Treatment should be directed by the patient’s main concerns. This may be pain, cosmesis or difficulties with footwear.
Non-operative management
Non-operative management options are summarised in Box 1. It is recommended that footwear be accomodative, with a wide, deep toe box and a low heel. Referral to a podiatrist for shoe stretching or modifications may assist patients in wearing their desired footwear, and it is particularly useful for patients with associated peripheral vascular disease or diabetes who may be at increased risk of skin breakdown. Padding over the medial eminence with an over-the-counter bunion cushion may provide symptomatic relief. There is some evidence to support orthotics, toe spacers, splinting and braces, which may provide symptomatic relief and decrease pain in some patients.9–13 Unfortunately, the available literature on the use of orthotics is limited, and no strong conclusions can be drawn regarding their use. If they do lead to improvement in symptoms, this effect is unlikely to last long term.9 It is also important to note that correction of the deformity will not occur with braces or splinting.12,13 For patients who complain of transfer metatarsalgia, a metatarsal dome may help offload the lesser toe metatarsal heads. Orthotics to address associated pes planus in paediatric patients may also relieve bunion pain.3
| Box 1. Non-operative management options for bunions |
- Nonsteroidal anti-inflammatory drugs
- Accommodative shoe with wide toe box and low heel
- Shoe stretching
- Bunion splints/braces
- Orthotics – medial arch support, metatarsal dome
- Toe spacers
|
Anti-inflammatory medications are recommended for pain relief.14 However, given the increased prevalence of bunions with increasing age, comorbidities such as renal impairment and peptic ulcer disease may preclude their safe use. Opioid medication should be avoided wherever possible.
It is important to note that non-operative management may not be successful in all patients. While there have been individual studies showing symptomatic relief with non-operative management, a Cochrane review published in 2004 found no difference when compared with no treatment at all.15 A trial of non-operative management is still advised, and may be of particular use for adolescent patients, those awaiting orthopaedic review and patients unfit for, or not desiring, surgery.
Operative management
There are >100 operations described for treating bunions.16 The type of procedure performed is dependent on the severity of deformity, as well as the surgeon’s preferences. Most patients will undergo some form of corrective osteotomy (Figure 2), with or without an additional soft tissue procedure. The chevron and scarf osteotomies are both commonly used in Australia. Mild-to-moderate deformities are generally treated with a distal metatarsal osteotomy, and more severe deformities may require a proximal osteotomy or tarsometatarsal joint fusion. If there is severe arthritis (hallux rigidus), an MTPJ fusion may be indicated. Simple resection of the bony prominence (bunionectomy) is rare, as there is a high recurrence rate and patients are usually dissatisfied with the outcome.16 Soft tissue procedures are also rarely performed in isolation and are more commonly used as an adjunct to osteotomy.16 Minimally invasive surgery techniques are increasingly being used; however, the majority of studies show no difference in patient function, complication rates and clinical outcomes when compared with standard techniques.17
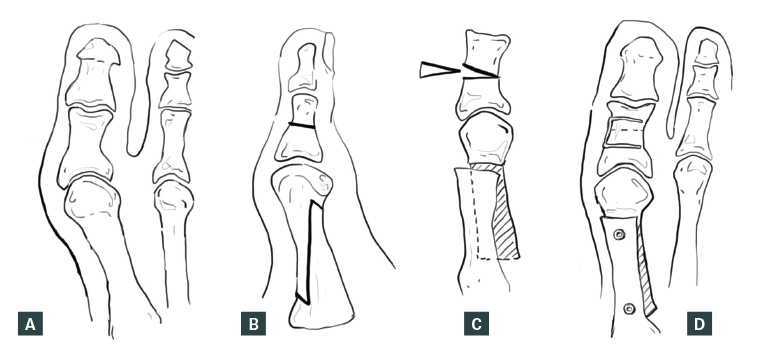
Figure 2. Corrective osteotomy (scarf and akin procedures)
A. Preoperative deformity; B. Osteotomy cuts; C. Realignment of metatarsal and closing wedge osteotomy of proximal phalanx; D. Fixation
Referral to an orthopaedic specialist is recommended if the patient has a painful prominence, has exhausted non-operative management and is a suitable operative candidate. The degree of functional impairment experienced and co-existing medical conditions are other considerations when deciding to refer. Patients with rheumatoid arthritis and diabetes may have additional foot concerns that require treatment. An examination of the lower limb and foot should be performed, as well as a simple gait assessment. Careful attention is required for overlying skin in patients with risk factors for breakdown and wound complications such as peripheral vascular disease and diabetes. If there is impending skin breakdown or ulceration, a more urgent referral is recommended. Juvenile bunion is one scenario in which delaying surgical intervention may be appropriate, as this should be avoided where possible until the patient reaches skeletal maturity.3 Delaying surgery decreases the risk of recurrence and avoids damage to open growth plates,3 but this needs to be considered against the progression of deformity and possible later requirement of a more extensive correction. Referral can still be made; however, early surgery may not be offered. Weight-bearing anteroposterior, oblique and lateral foot radiographs should be performed. Arterial dopplers and diabetic screening can also be considered prior to referral.
It is important to note that cosmesis alone is not an indication for operative management. Relief of pain is the main goal of surgery. While improved appearance and ability to wear desired footwear are secondary goals, a significant percentage of patients will still have difficulties with footwear following surgery, and some will still have cosmetic concerns.9,18 Smoking is also a relative contraindication to surgery and is associated with increased wound complications, delayed union following osteotomy and poorer patient-reported outcomes.19–21 Smoking cessation should be strongly encouraged.
Following surgery, weight-bearing is allowed in a stiff-soled post-operative shoe, which is required for six weeks. Driving is not permitted until the patient has been cleared to return to normal footwear.
Conclusion
Bunions are a common forefoot condition, with increased prevalence in the female population and increasing prevalence with age. Non-operative management is centred on appropriate footwear, simple analgesia and orthotics, splints/braces and toe spacers. These have all been shown to reduce pain and provide symptomatic relief. The natural history of bunions is of progression, and patients are unlikely to obtain long-term pain relief or resolution of symptoms with non-operative management.
Once non-operative management has been exhausted, referral to an orthopaedic specialist is recommended. However, paediatric and adolescent patients with juvenile bunion may not be offered early surgical intervention, as this should be delayed until skeletal maturity where possible. Many patients will have concerns regarding cosmesis, but this alone is not an indication for surgery. The goal of surgery is pain relief, and cosmetic concerns and footwear difficulties may persist despite a successful operation. The type of surgery is dependent on the degree of deformity and surgeon’s preference. Most patients will undergo some form of corrective osteotomy, and smoking cessation is important for this to heal.
Key points
- Bunions are a common forefoot condition resulting in a progressive, painful deformity at the MTPJ.
- Non-operative management is centred on appropriate footwear, splints/braces, toe spacers, orthotics and simple analgesia.
- Referral to an orthopaedic surgeon is recommended if the patient complains of a painful prominence, has exhausted non-operative management or has impending skin breakdown or ulceration.
- Delayed surgical intervention may be appropriate in cases of juvenile bunion as surgery should be avoided until the patient reaches skeletal maturity, if possible.
- Pain relief is the primary goal of surgery, and patients may still have some cosmetic or footwear concerns despite a successful operation.