Feature
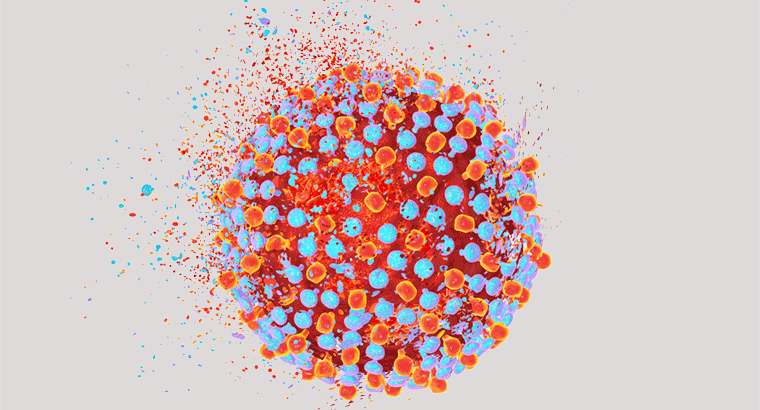
Hepatitis C: Eliminating stigma and boosting treatment
Stigma is the greatest barrier preventing people from receiving life-saving treatment for viral hepatitis.
 Stigma is a strong barrier to treatment for many patients.
Stigma is a strong barrier to treatment for many patients.
Nearly 1000 Australians die each year from hepatitis B and C. Many of these deaths are attributable to liver cancer, which can be caused by chronic viral hepatitis infection and is one of the fastest rising causes of cancer death in Australia.
But since March 2016, when the Federal Government subsidised and made available on the Pharmaceutical Benefits Scheme (PBS) a range of direct-acting antivirals with a 90–95% cure success rate, hepatitis C-related deaths are far more preventable. Yet despite an initial rush for treatment, numbers of patients accessing the direct-acting antivirals have slowed.
Research has found that what stops many of these potential patients from accessing health services is stigma arising mostly from the association of hepatitis C with injecting drugs.
‘Stigma is a major barrier that stops people getting tested and treated, resulting in potentially deadly consequences,’ Melanie Eagle, CEO of Hepatitis Victoria, said.
‘Many choose not speak openly about their hepatitis status out of fear of being treated differently by family, friends, and professionals.’
To combat this, Hepatitis Victoria is marking March 1 – Zero Discrimination Day – by launching a 12-part series of short videos called ‘Stigma Stories,’ to be released monthly. The videos feature people with hepatitis C describing their experiences with discrimination as a result of their disease in many different quarters of life – including in encounters with healthcare providers.
Dr Annie Balcomb, a GP with a special interest in viral hepatitis, has encountered similar stories among her own patients.
‘I think [people with hepatitis C] are a marginalised group, on the whole,’ she told newsGP. ‘The majority are no longer using, but they seem to get labelled and put into a basket.’
Dr Balcomb believes that stigma can also prevent health professionals from realising there may be potential cases of hepatitis C in their own waiting rooms.
‘There’s a lot of people from all stratas of society who used [injecting drugs] maybe once or twice or for a year of their life,’ Dr Balcomb said.
‘So it’s important to try and de-stigmatise hepatitis C and make people feel comfortable. GPs can put a poster up in their rooms [about hepatitis C treatment] and also consider it for testing and find someone they can refer to.’
Dr Balcomb would like to see GPs fight the stigma against hepatitis C and embrace that they have a key role in eliminating the disease in Australia.
‘I would love to see [hepatitis C treatment] become a priority for a push from all GPs across Australia, it’s the most revolutionary thing,’ she said. ‘We’re aiming to eliminate Hepatitis C from Australia by 2028, 2030 at the latest.’
direct-acting-antivirals hepatitis-C
newsGP weekly poll
Is it becoming more difficult to access specialist psychiatric support for patients with complex mental presentations?