Column
Old doc, new drugs: Glifozins
Dr Casey Parker examines a newer class of drugs for diabetes.
 Is it worth switching to the newer class of diabetes drugs?
Is it worth switching to the newer class of diabetes drugs?
Quick confession before we get started: I have never read or seen anything about Harry Potter in my life.
It’s not because I am opposed to the Rowling machine. I just grew up at the time before Harry and then had kids who missed the last few episodes. I guess I have a lot to look forward to one day when my boys go wizard-crazy?
The reason I bring this up is that I imagine that if J.K. Rowling was going to name a class of drugs, then she would choose the title ‘gliflozins.’ Awesome name for a magical potion, weird name for an actual drug.
As an ED doctor, I know about as much about these gliflozins as I do about Hogwarts’ pupils. They are a mysterious new entity that has started turning up on medication lists in recent years. So I am going to take a look at this class of drugs and try to work out where they fit into the diabetes oeuvre.
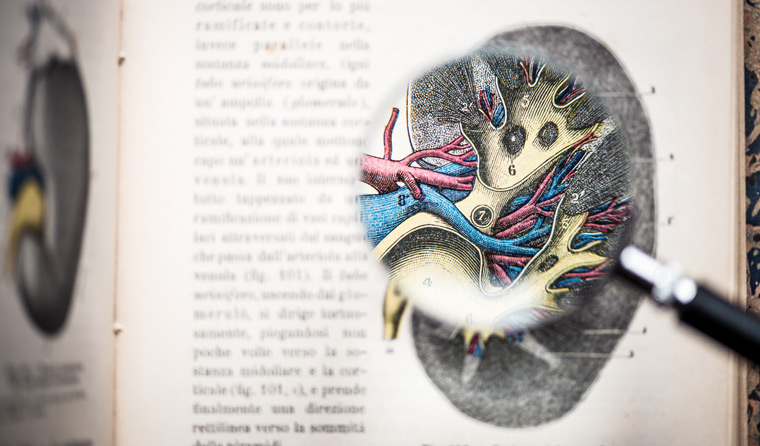
SGLT2 protein
The ‘gliflozins’ are SGLT2 inhibitors. The sodium-glucose co-transporter is a protein that lives on the proximal convoluted tubules in one’s kidneys (presumably the ‘2’ indicates ‘the later model’).
The main job of the SGLT2 protein is to reabsorb glucose that has been excreted in the glomerulus, and hence bring it back into the plasma. It also pumps sodium back into the circulation.
In people with diabetes, who are already hyperglycemic, the SGLT2 protein is upregulated to cope with all the sugar hitting the tubules.
As the little pumps try to reabsorb the excess glucose, they also bring back sodium and water, therefore contributing to hypertension and possibly fluid overload. Hence this is a neat target for the treatment of diabetes.
Importantly, the SGLT2 protein is not dependent on insulin, so it works and can be inhibited without affecting or being affected by the pancreatic hormones.
The actual molecule upon which the gliflozins are based, phlorizin, has been known about for a long time (it was first isolated in 1835). However, the current generation of molecules was not released onto the market until quite recently.
There was a lot of effort to try to find drugs that specifically inhibited the SGLT2 protein. Turns out that inhibiting the SGLT1 protein gives the patient iatrogenic, choleriform diarrhoea, which is a tough thing to market.
The current crop of SGLT2 inhibitors includes ertugliflozin, canagliflozin, empagliflozin and dapagliflozin. Since these are all tough to say and sell, the creative folk in the pharma companies decided to give them names like Invokana, Jardiance, Stegaltro and Forxiga.
Canagliflozin (Invokana) got a divorce from the Pharmaceutical Benefits Scheme (PBS) in 2015 and is no longer available in Australia.
The mechanism of action of SGLT2 inhibitors is reasonably straightforward. They stop your kidneys reabsorbing the glucose that gets filtered and you end up passing it into the urine and out into the world. This tends to reduce the plasma glucose load and decreases the stimulation of the pancreatic beta-cells to produce more insulin. It also means your body is getting rid of calories via the urine.
So the urine is now sweeter and a little saltier and, voila, your patient is peeing margaritas.
Of course, this does have a few downsides. Let’s have a look at those.
Downsides
The most common side effect of SGLT2 inhibitors is urogenital infections. All of that extra sugar provides a happy medium for bacteria and fungi. There is a risk of urinary tract infection (UTIs), vulvovaginitis, candida and rarely Fournier’s necrosis of the perineum (aka necrotising fasciitis, which is very unpleasant).
All of the extra excreted sugar (and salt) tends to create an osmotic drag, which can lead to dehydration. There is also the problem of urinary frequency and the need to get up at night to empty the bladder, orthostatic hypotension and possibly falls.
The risk of acute kidney failure is also increased – likely as a result of relative hypovolemia in patients with vulnerable beans to begin with. In our hot Australian climate, this might be a big issue.
There are also a few very serious potential effects of SGLT2 inhibitors.
The first one to mention is the recent post-marketing association with increased risk of toe and lower limb amputations. The US Food and Drug Administration (FDA) placed a black box warning on canagliflozin for amputation risk. A recent study showed the risk was roughly doubled compared to patients taking other diabetic medications. This appears to be a class effect, as this study included patients taking gliflozins other than canagliflozin.
The gliflozins can also produce euglycemic diabetic ketoacidosis. That is ketoacidosis in the presence of a normal blood glucose level. This is an important factoid for the emergency doctors out there. We need to be checking the finger-prick blood sugar levels (BSL) and ketones in patients who are prescribed gliflozins. Don’t be reassured by a normal sugar.
Okay, so now the big question
Do they actually work? Are they saving lives? That is really what we want to know when we decide whether or not to use these drugs.
As with any new drug, the trials that attempt to answer this question are conducted by the drug companies that manufacture them. So these trials need to be taken with a pinch of salt (for example, the amount that might frost the rim of your margarita).
There are three big pharma-run trials – EMPA-REG, CANVAS and DECLARE-TIMI58 – looking at three different gliflozins. Just last week The Lancet published a meta-analysis and systematic review that combined all the data from these trials (34,322 patients followed for between 2–4 years) into one big punchbowl of data.
You can get a pretty good overview of the effects by reading that paper … or you can trust me and I will give you the headline outcomes. They are broken down into primary and secondary prevention.

Dr Casey Parker has found current data would suggest these drugs are best used in patients with established cardiovascular complications.
Here we go.
All-cause mortality was better in patients taking a SGLT2i. About a 15% reduction if you take all comers.
In patients with an atherosclerotic cardiovascular disease, the hazard ratio was 0.83 (0.75–0.92).
In those with pre-disease risk factors, the hazard ratio was 0.90 (0.77–1.05), ie not significant.
For the composite outcome (a bit statistically naughty) of myocardial infarction, stroke or cardiovascular death, there was:
- a benefit for patients with diagnosed cardiovascular disease (ie secondary prevention)
- no benefit for patients with no known cardiovascular disease (primary prevention).
The same was observed for ‘hospitalisation for heart failure’ or cardiovascular death.
A benefit in people with a disease, no benefit in folk without diagnosed diseases of the vessels. Physiologically, this makes sense. We would expect a reduction in heart failure on these drugs.
You may be seeing a theme here. SGLT2 inhibitors seem to work in people with actual diagnosed heart disease. The data for primary prevention is really not showing a benefit.
The only outcome that seemed to show the most benefit to all patients was for reduction of renal failure, progress to end-stage renal failure and renal death, with nearly a 50% effect size by this measure. So the kidneys are one area where these drugs may be more useful.
The authors of this meta-analysis conclude, somewhat counterintuitively, that we ought to consider SGLT2 inhibitors in all people with diabetes, regardless of the actual presence of established cardiovascular disease.
I believe that is a bridge too far. Like all things in medicine, there is a balance between harms and benefits. The side effects are not insignificant and, with time, the ‘real world’ harms will start to be reported. The pre-market evidence always underestimates the downsides.
For me, the current data would suggest these drugs are best used in patients with established cardiovascular complications. They may also be useful in folk with heart failure and progressing renal disease.
Okay, that’s a wrap. I am off to the cocktail bar for a lime margarita.
This article is adapted from Dr Casey Parker’s blog, Broome Docs.
Update: The original version of this article incorrectly listed ‘heart rate’ instead of ‘hazard ratio’ when discussing patients with an atherosclerotic cardiovascular disease.
diabetes glifozin Old doc new drug
newsGP weekly poll
What is your chief concern with role substitution?