News
Remdesivir and COVID-19: What GPs need to know
It has become the first therapy for COVID-19 to receive FDA approval for emergency use – but evidence of its effectiveness remains mixed.
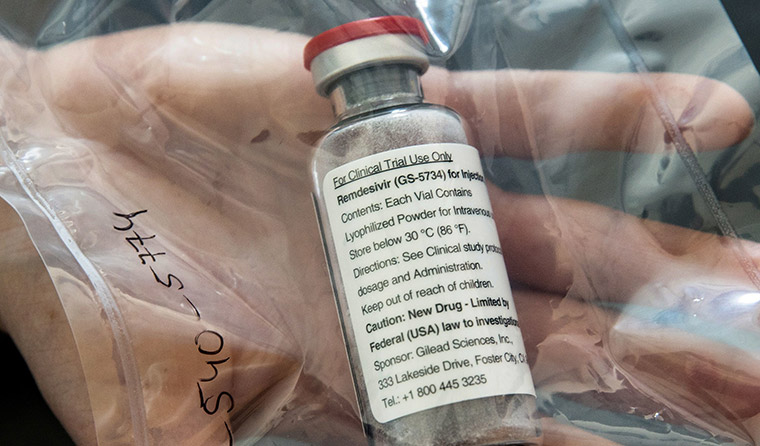 Remdesivir is a nucleoside analogue prodrug that has inhibitory effects on pathogenic animal and human coronaviruses, including SARS-CoV-2 in vitro. (Image: AAP)
Remdesivir is a nucleoside analogue prodrug that has inhibitory effects on pathogenic animal and human coronaviruses, including SARS-CoV-2 in vitro. (Image: AAP)
It has been hailed as a major development in the global fight against COVID-19, but what is remdesivir?
‘It’s promising.’
That is infectious diseases physician Associate Professor Steven Tong from the Royal Melbourne Hospital and the Doherty Institute.
He is talking to newsGP about the potential use of remdesivir as a treatment for COVID-19.
Remdesivir is a nucleoside analogue prodrug that has inhibitory effects on pathogenic animal and human coronaviruses, including SARS-CoV-2 in vitro.
It was originally developed to treat Ebola.
Research published on 17 March found remdesivir can potentially act as a SARS-CoV-2 RNA-chain terminator, effectively stopping its RNA reproduction.
The drug has shown promise against COVID-19 in animal model trials, and in some small human trials.
What is happening in Australia?
The Guardian reported on 1 May that five hospitals in Australia are set to receive remdesivir.
The only confirmed location is St Vincent’s Hospital in Sydney.
Associate Professor Tong said the drug is not being used in Australia as part of a clinical trial.
‘My understanding is that it is for compassionate use,’ he said. ‘Obviously, Gilead [the makers of remdesivir] don’t have enough drug to supply everyone with it.
‘My understanding is they’re going to prioritise areas of the world where there’s a lot of COVID at the moment, and that what will be provided to Australia will be fairly limited – potentially only five hospitals – which obviously doesn’t cover much of our population.’
Associate Professor Tong said the drug will only be given to COVID-19 patients who are in intensive care.
What does the research show?
Associate Professor Tong said examining data relating to remdesivir is currently challenging.
‘It’s obviously a difficult space because there’s so much data coming out in such different ways, [including] by press release, which isn’t ideal,’ he said.
The two main trials that have recently been in the spotlight include one that is still underway, known as the Adaptive COVID-19 Treatment (ACTT) trial, and one published in The Lancet.
The ACTT trial
Preliminary results from this trial, published on 29 April, found that hospitalised patients with advanced COVID-19 and lung involvement who received remdesivir had a 31% faster recovery time than similar patients who received a placebo.
Specifically, the median time to recovery was 11 days for patients treated with remdesivir compared with 15 days for those who received a placebo.
The randomised controlled trial involves 1063 patients and began on 21 February.
The trial has been sponsored by the US National Institute of Allergy and Infectious Diseases (NIAID) and is also referred to as the National Institute of Health (NIH) trial.
Results also suggested a survival benefit, with a mortality rate of 8% for the group receiving remdesivir versus 11.6% for the placebo group – but the trend was not statistically significant.
Speaking on 29 April, Dr Anthony Fauci, head of the US National Institutes of Allergy and Infectious Diseases, said the data of early results from this study showed a ‘clear-cut, significant, positive effect in diminishing the time to recovery’.
Dr Fauci said the results were so promising, there was ‘an ethical obligation to immediately let the placebo group know so they can have access’ to the drug.
‘What it has proven is that a drug can block this virus,’ Dr Fauci said.
The final results of this trial are not expected until the end of May.
Associate Professor Tong agrees this study shows promise.
‘We will need to wait and see the actual data itself, but the reduction in time to clinical recovery looks like it’s significant,’ he said.
Associate Professor Tong called the change in mortality ‘nearly significant’.
‘Obviously that’s what [Dr Fauci has] presented, but it’s just really hard to make a firm comment at this stage without seeing the actual data itself.
‘Hopefully we’ll see that in the next two to three weeks.’
Infectious diseases physician Associate Professor Steven Tong believes the use of remdesivir for COVID-19 is ‘promising’.
A further development: FDA authorises emergency use of remdesivir to treat COVID-19
The US Food and Drug Administration (FDA) in the US authorised the emergency use of the drug for treating COVID-19 on 1 May.
‘Given there are no adequate, approved, or available alternative treatments, the known and potential benefits to treat this serious or life-threatening virus currently outweigh the known and potential risks of the drug’s use,’ the FDA wrote in a press release.
The FDA action specifies the drug may be used for adults and children with suspected or confirmed COVID-19 diagnoses who are severely ill with low blood-oxygen levels or who may be on a ventilator.
The Lancet trial
A randomised, double-blind, placebo-controlled study was published in The Lancet on 29 April.
It was a multicentre trial at 10 hospitals in Hubei, China, involving 237 hospitalised patients with laboratory-confirmed SARS-CoV-2.
Those patients were randomly assigned in a 2:1 ratio to intravenous remdesivir (200 mg on day one, followed by 100 mg on days 2–10 in single daily infusions) or the same volume of placebo infusions for 10 days.
Patients were permitted concomitant use of lopinavir–ritonavir, interferons, and corticosteroids.
The research found remdesivir use was not associated with a difference in time to clinical improvement.
It also found that patients receiving remdesivir had a numerically faster time to clinical improvement than those receiving placebo among patients with symptom duration of 10 days or fewer – but this finding was not statistically significant.
Meanwhile, adverse events were reported in 102 of 155 remdesivir recipients (66%) versus 50 of 78 placebo recipients (64%).
Remdesivir was stopped early because of adverse events in 18 patients (12%) versus four patients (5%) who stopped placebo early.
While these results do not seem promising, Associate Professor Tong said the confidence interval in this study sits within the confidence interval of the more hopeful, ACTTtrial.
‘So it is possible that if The Lancet study continued to a larger sample size, they may have come to a similar conclusion,’ Associate Professor Tong said.
‘We’ll never actually know that.’
Potential adverse effects of remdesivir
On 29 April, US biopharmacetical company Gilead Sciences announced the results from the open-label Phase 3 trial of investigational remdesivir in patients with severe COVID-19.
It found that patients receiving a 10-day treatment course of remdesivir achieved similar improvement in clinical status compared with those taking a five-day treatment course.
That trial also explored adverse events.
Gilead noted the most common adverse events occurring in more than 10% of patients in either group as nausea, acute respiratory failure, and grade three or higher alanine aminotransferase (ALT) elevations on liver enzymes.
Three per cent of patients in this study discontinued treatment with remdesivir due to elevated liver tests.
Associate Professor Tong said it is important to watch this space as the completed data from the ACTTtrial emerges in the coming weeks.
‘At the moment, I’d just summarise [by saying] it’s promising,’ he said.
‘But let’s wait for the full data before we make any conclusions.’
Log in below to join the conversation.
antiviral drug coronavirus COVID-19 remdesivir
newsGP weekly poll
Is it becoming more difficult to access specialist psychiatric support for patients with complex mental presentations?