Opinion
Old doc, new data: Canaglifozin
Can-I-get-a-flozin? Dr Casey Parker examines new evidence for the diabetes medication.
 Second line oral diabetes agent canaglifozin was withdrawn from the PBS. Should that change?
Second line oral diabetes agent canaglifozin was withdrawn from the PBS. Should that change?
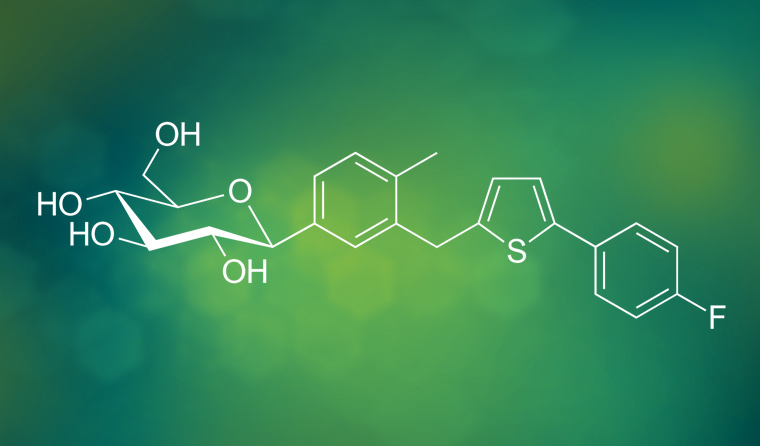
A while back, I wrote a piece on the sodium-glucose transport protein 2 (SGLT2) inhibitors, the flozin drugs, in which I noted that canagliflozin had been vanquished by the Pharmaceutical Benefits Scheme (PBS).
While my understanding of the inner workings of the PBS is admittedly limited, from what I can tell, here’s what happened.
In 2012, canagliflozin (sold as Invokana) was listed on the PBS as a second-line oral diabetes agent. Manufacturer Janssen–Cilag was smitten with the drug, and the pair dated happily for a while.
Over the next few years, however, a few other newer, cheaper SGLT2 agents got the attention of the PBS. So the PBS went back to Janssen–Cilag, saying, ‘We have started seeing other SGLT2 agents. Can you drop your price?’
Janssen–Cilag decided it wasn’t worth the hassle and yanked canagliflozin from the market in 2015.
This amicable breakup seemed to be going well until just last month. Canagliflozin was back, with an evidentiary facelift, renal ‘filler’ and cardiovascular collagen injections. I believe it is quite likely that the PBS will have to rethink its position on the situation.
The new evidence? The CREDENCE trial (Canagliflozin and renal outcomes in type 2 diabetes and nephropathy), published in the New England Journal of Medicine in April. It is being hailed as the best thing since sliced (low-GI, wholemeal) bread for people with diabetes who have renal disease, and certainly has a lot of endocrinologists, cardiologists and renal physicians a bit hot under the collar.
Clinicians treating diabetic nephropathy have been somewhat desperate for many years. It has been a long time since their last night out with the angiotensin-receptor blockers.
So, is the hype deserved? What was this ‘miracle’ trial all about and what do the numbers really tell us about canagliflozin in 2019? Let’s take a good look.
Before and after
George Clinical group, which conducted the new trial, previously published the CANVAS and CANVAS-R (canagliflozin and cardiovascular and renal events in type 2 diabetes) trials in 2017. These earlier trials included more than 10,000 people with diabetes in the first trial, with the ‘R’ (for renal) arm including 5812 patients with nephropathy, although not with exactly the same inclusion criteria as CREDENCE.
In CANVAS-R there was a significant reduction in progression of renal disease. However, the renal outcomes were only part of the secondary analysis in CANVAS. There was also a raft of undesirable side effects. A new trial is good science in such situations, particularly when designed to look specifically at the hypothesis generated by earlier data. CREDENCE was thus hatched.
CREDENCE is a double-blind, randomised trial, with 4401 people with type 2 diabetes who had albuminuric chronic kidney disease recruited from 34 different countries.
To be included, patients needed to have:
- estimated glomerular filtration rate (eGFR) of 30 to <90 (ie CKD3 or better)
- albuminuria (ACR >300 to 5000)
- ongoing treatment with renin–angiotensin system blockade.
As part of the trial, participants received either 100 mg canagliflozin daily or a placebo. As expected, placebo patients were on a well-stuffed blister pack of other drugs.
The groups were equal at entry, as you would expect from such a large cohort.
The primary outcome was a composite (which is not what we like to see), including:
- end-stage kidney disease
- doubling of the serum creatinine level
- renal or cardiovascular death.
The trial stopped recruiting patients earlier than expected, as they reached the predetermined number of events after 4200 patients had been followed for an average of 2.62 years. There was a high rate of dropout at 27%.
So what’s the big deal?
The headline result that got everybody excited was a 30% relative risk reduction in the overall composite primary outcome.
Breaking it down, there was a significant reduction in all the lab-based outcomes and requirement for renal replacement. Importantly, there was no difference in the mortality outcomes either overall or in disease-specific deaths. The
number needed to treat (NNT) for the primary outcome was 23.
CREDENCE did not find the same rates of adverse events as were problematic for the CANVAS cohorts.
There were increases in urogenital infections, as in previous SGLT2 trials. The number needed to harm (NNH) was 59.
Amputation rates in CANVAS were twice as high as in CREDENCE, making it an insignificant finding in the new trial. This could be because of the higher doses allowed in CANVAS – up to 300 mg of canagliflozin.
We will need to look at this issue more closely in the future, given the trial stopped early and will, therefore, underestimate late harms such as these.
In real life practice, patients will be titrated up to a 300 mg dose, at which point amputations may be a real side effect.
Osmotic diuresis and volume depletion were significant adverse findings in CANVAS. Interestingly, however, they were not reported specifically in CREDENCE. This could be a significant issue if your patient lives in the warmer climes of Australia.
There was a very small increase in risk for diabetic ketoacidosis (DKA) in CREDENCE, which was developed by half of 1% of patients in the canagliflozin group. This rare but serious effect should be noted, especially when patients are sick or undergoing surgery, where we need to be aware of the risk of so-called
euglycemic DKA. The
Australian and New Zealand College of Anaesthetists currently recommends withholding SGLT2 inhibitors for a three-day period prior to surgery.
To summarise
CREDENCE showed that a daily 100 mg dose of canagliflozin reduces the kidney-specific outcomes in people with diabetes who have existing nephropathy. The data shows a slowing of the normal decay we see in diabetic kidney disease.
This is big news.
It has been a long time since we had a new therapy that might prevent our patients with diabetes from ending up on dialysis. I believe this is a practice-changing trial for patients meeting the inclusion criteria.
As one caveat, though, the safety of canagliflozin remains a bit of an issue for me. Although CREDENCE showed much less harm than previous trials, I am still a bit sceptical.
This latest trial was the smallest and had the shortest follow up. Looking at the data, it’s clear there was a very high rate of drop out and non-adherence in these trials. This does muddy the waters when it comes to estimating the harms of this drug.
If we are going to adopt this drug, we need to remain vigilant and watch for urinary-tract infections, DKA, volume issues and foot problems in patients with diabetes.
No drug is perfect; they all have a few quirks. However, I do feel this could be the start of a beautiful relationship.
canaglifozin diabetes pharmaceutical benefits scheme
newsGP weekly poll
What is your chief concern with role substitution?