In Australia, over two-thirds of the adult male population and half of the adult female population are overweight or obese,1 with obesity defined as a body mass index (BMI) ≥30 kg/m2.2 Given the high disease burden from obesity, bariatric surgery is considered a viable option as it results in effective long-term weight loss.3,4 Indications for bariatric surgery according to National Health and Medical Research Council (NHMRC) criteria are morbid obesity (BMI ≥40 kg/m2) or a BMI ≥35 kg/m2 with obesity-related comorbidities.
Laparoscopic sleeve gastrectomy (LSG) is a type of bariatric surgery that involves removing part of the stomach via a laparoscopic procedure. Until 2004, LSG was not performed as a stand-alone procedure in Australia.5 However, it is now recommended as an effective procedure for weight loss, with recognised reduced mortality and improvement in comorbidities.4 While the long-term metabolic benefits of LSG are now established,6,7 the broader physical effects of the surgery, as well as its psychosocial impact, have been less explored. The impact of other forms of bariatric surgery on patients’ lives goes beyond metabolic improvements,8 and the authors of this article believe that LSG offers similar wide-reaching benefits. However, surgery is an irreversible and elective procedure; therefore, healthcare providers need to be cautious when recommending it. There may be unidentified negative consequences of the surgery that are not accounted for by either patients or healthcare providers. Full consequences experienced by patients should be considered by the healthcare providers who recommend, perform and support patients choosing to have surgery.9 While there has been international research into patient experiences post–bariatric surgery, there is limited published data on the Australian context. It is important to note that the Australian healthcare system differs from other countries, with LSG being reasonably easy to access through the private healthcare system. However, fitting the NHMRC criteria and being able to access private health cover easily does not guarantee a successful outcome.
The purpose of this study was to elucidate aspects of the Australian patient experience following LSG. Their stories were explored with wide-ranging discussions regarding their psychosocial functioning, exercise habits, relationships and overall satisfaction/dissatisfaction with their lives.
Methods
A mixed-methods approach was chosen to explore the breadth and depth of patient experiences, including any unforeseen topics that might be revealed in the qualitative interviews. Ethics approval was obtained through the Bond University Ethics Research Committee – protocol number 0000015647. The research team comprised a general practitioner (NY), six Doctor of Medicine (MD) students (AK, ShS, FK, YT, DG and AC) and a bariatric surgeon (VL). VL performed the surgery; none of the other researchers had any relationship with the participants.
Data collection
The data collection process is shown in Figure 1. All patients who underwent LSG at Gold Coast Private Hospital with a single surgeon, between April 2013 and March 2016 (total 284), were divided into three groups according to how long ago they had their surgery: one, two or three years ago. Participants were then selected from each year group using a computerised random number generator, with 34 patients from each group chosen (year one, two and three post-operative). A total of 102 invitations to participate were posted, including an explanatory statement, consent form and reply-paid envelope. The consent form included a request for their preferred contact email and telephone number, which was used thereafter to connect with the participants. Letters were followed up with separate email reminders at one and two months. Excluded were patients who had had prior bariatric surgery (ie laparoscopic band), conversion to open surgery, or a known hiatus hernia.
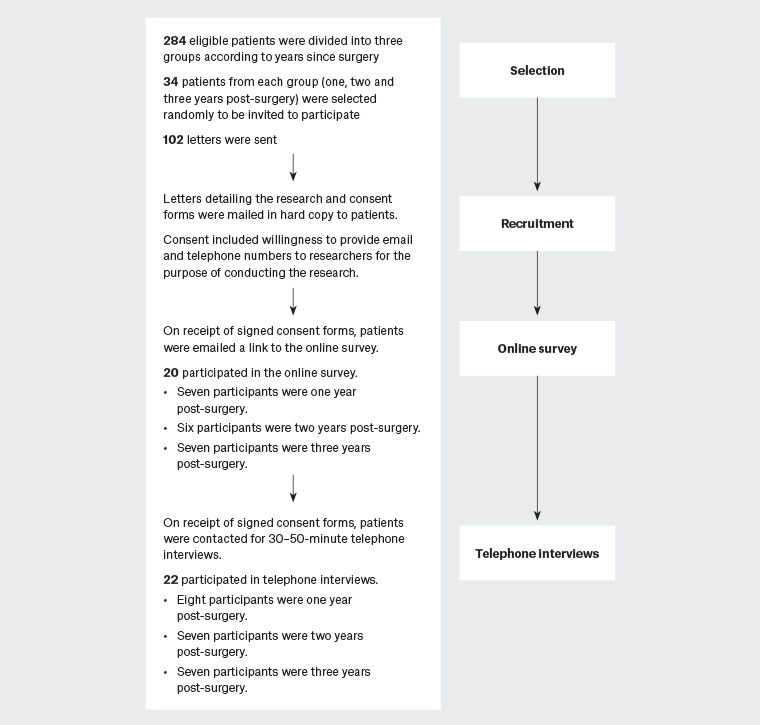
Figure 1. Data collection method outline
Once the signed consent form had been returned (in paper format), patients were emailed a link to an online Qualtrics survey that collected quantitative data including demographic data, degree of weight loss, motivating factors for surgery, side effects of surgery, exercise, diet, social relationships and changes since surgery.
Qualitative data were then collected via recorded telephone interviews. Two researchers (YT and AK) were trained to conduct the interviews by an experienced qualitative researcher in the faculty (SS), including practice interviews on a bariatric patient who was not involved with the study. Once it was believed that both researchers explored the patient’s experiences sufficiently similarly, they conducted approximately 30–50-minute semi-structured interviews over a two-month period with the 22 respondents. They explored the same list of topics as surveyed in the Qualtrics questionnaire, but used open-ended questions about the patients’ experiences, attitudes and behaviours so that their stories and voices were able to be heard. More than 12 hours of interviews were conducted, and the interview guide is available on request. Verbatim transcriptions were made by three members of the research team (FT, ShS and DG) and cross-checked by a different member to ensure fidelity. All 22 interviews were conducted before data analysis so data saturation was not considered as a reason to truncate the number of interviews.
Data analysis
Quantitative data were extracted from the survey in TSV format and (where appropriate) analysed using an Excel spreadsheet.
Qualitative data from the semi-structured interviews were analysed inductively using thematic analysis. The theoretical framework for using thematic analysis as a method in its own right is argued by Braun and Clarke.10 This method was chosen because it is a flexible tool that can provide rich, detailed accounts of data. It is also accessible to students and those not particularly familiar with qualitative research. The research team included MD students who wanted to learn about performing qualitative research, hence it seemed a wise choice.
Thematic analysis was performed by four researchers (ShS, AC, DG and FK) under the guidance of SS. Data from half of the interviews were inductively coded by two teams, each consisting of two researchers. Each team coded a separate group of interviews and identified themes, statements or ideas that were then discussed and agreed on between the two groups. Potential and prospective categories were developed into codes, and then all transcripts were re-coded by all researchers according to the newly constructed framework.
Results
Of the 102 letters sent, 25 participants returned signed consent forms. Of these, 20 completed the survey and 22 undertook the telephone interview; eight were one year post-LSG, seven were two years post-LSG and seven were three years post-LSG.
Survey results
Of the participants, three were male and 19 were female, with ages ranging from 24 to 61 years (mean = 43.9 years). BMIs ranged from 35.2 kg/m2 to 55.2 kg/m2 (mean = 41.5 kg/m2). This is comparable to the general population of patients who undergo bariatric surgery, where females comprise 77.2% of procedures, the mean age at operation is 42.7 years and mean BMI is 42.2 kg/m2.11 Most participants had been diagnosed with at least one comorbidity prior to surgery (Table 1), and their motivations for having surgery were varied (Table 2).
Tables 3–6 summarise further relevant findings from the Qualtrics survey.
| Table 1. Comorbidities prior to surgery |
| Comorbidity |
% |
| Hypertension |
35 |
| High cholesterol |
30 |
| Gastro-oesophageal reflux |
10 |
| Type 2 diabetes |
10 |
| Obstructive sleep apnoea |
0 |
| None |
10 |
| Table 2. Motivations for having surgery |
| Motivation |
% |
| Wanted to live longer |
70 |
| Health concerns |
55 |
| Desired an increase in self‑confidence |
40 |
| To increase fitness and exercise endurance |
25 |
| Social pressures |
15 |
| Table 3. Other weight loss methods trialled prior to surgery |
| Weight loss method |
% tried |
| Exercise |
80 |
| Medication/diet pills |
75 |
| Weight loss groups |
75 |
| Herbal preparations |
50 |
| Diets* |
10 |
| *Twenty different diets/eating plans listed among participants |
| Table 4. Effect of laparoscopic sleeve gastrectomy on exercise |
| Effect on exercise |
Percentage of patients listing a moderate-to-high improvement |
| Desire to exercise |
50 |
| Exercise tolerance |
75 |
| Exercise frequency |
60 |
| Table 5. Effect of laparoscopic sleeve gastrectomy on diet |
| Effect on diet |
Percentage of patients listing a moderate-to-high improvement |
| Portion control |
100 |
| Helped to make better choices |
60 |
| Improved cravings |
50 |
| Table 6. Effect of laparoscopic sleeve gastrectomy on relationships |
| Effect on relationships |
Percentage of patients listing a moderate-to-high improvement |
| Improved enjoyment when engaging with family and friends |
90 |
| Engaged with new social activities or hobbies |
65 |
| Felt more comfortable in social situations |
85 |
Overall, 90% of participants stated that they were ‘extremely satisfied’ with the effect of the surgery on their life in general. The remaining 10% stated they were ‘slightly satisfied’; no one was neutral or dissatisfied.
When comparing the three groups (one, two and three years post-surgery), there were no significant differences across any of the explored parameters.
Qualitative results
Thematic analysis of the 22 transcripts identified three overarching themes about patients’ experience of life after undergoing LSG:
- normality
- control
- ambivalence.
These themes were reflected in eight organising sub-themes:
- weight and health
- physical changes and daily living improvements
- exercise and fitness
- emotional responses
- eating behaviour and relationship with food
- societal influences
- body image
- relationships.
The theme of normality was expressed as finding a ‘new normal’, and many participants discussed how they needed to rethink their behaviours and attitudes across the subthemes.
The theme of control conveyed the overarching personal power that they now felt to positively influence the subthemes.
The theme of ambivalence was also shown across all the subthemes as participants articulated their struggles as well as successes.
Subthemes
1. Weight and health
Seeing the numbers on the scales go down after the surgery was motivating for patients.
I think it is the euphoria where you are so big and you suddenly drop 50 kg in 12–18 months and you are like, oh my god. (BR, three years post-LSG, female)
However, most patients also emphasised that the actual kilogram number was not their primary focus; they were more concerned about the improvement in their comorbidities and longevity.
[My wife] was always worried that I was going to die of a heart attack, and now the doctor thinks that I might outlive her. (JT, one year post-LSG, male)
2. Physical changes and daily living improvements
Some changes were functional and experienced in day-to-day life, while others were more about appearance.
I think things are cheaper for my size. Iam not eating as much. [The] weekly ... grocery shop is cheaper. Entertainment – eating out at restaurant, drinking and going out is definitely cheaper. (CL, one year post-LSG, female)
[B]eing able to sit on a bus chair and not have your flabby side hanging on your side. So socially being more like a normal-sized person, size 12–14. (BR, three years post-LSG, female)
There is hair loss. I knew that would happen. I have got sort of a thick hair so it has not affected me. You do lose a lot of hair. But it has stopped now … it was in the first six months. After that six-month mark, it was good. Everything has settled down. (CL, one year post-LSG, female)
3. Exercise and fitness
The effect on exercise habits was marked in most patients, with both a change in attitudes and in habits.
It sort of feels … more like I want to exercise most of the time. I’ve even started exercise I had never thought I would be able to do. (UM, two years post-LSG, female)
I don’t really see [exercise] as a chore now, whereas before it was like a huge chore, pretty much struggling to do anything effectively. (PR, three years post-LSG, female)
I think surgery definitely [motivated me to exercise]. I knew I had to exercise and I had to work hard to get the weight off. (JO, three years post-LSG, female)
A number of patients described taking up new sports, or rejoining sports they had enjoyed in their youth.
Just gotten back from the Kokoda trek in Papua New Guinea … that’s a milestone for me. (KE, three years post-LSG, male)
Other fitness activities mentioned by a range of participants included jet skiing, Pilates, CrossFit, ballroom dancing and belly dancing, netball, skateboarding, snorkelling and softball.
It seems therefore that patients increased their exercise post-operatively both in frequency and variety, partly because they knew it was an important part of the process but also because they noticed that exercise improved their energy and fitness.
4. Emotional responses
Two main fears were articulated.
1. Fear of returning to obesity:
My biggest fear is gaining that weight back. (NC, two years post-LSG, female)
2. Fear of judgement from society regarding the surgery:
Some people are very anti-surgery and those means of losing weight copped a bit of flack with a few people. (GE, one year post-LSG, female)
There was a clear description by most participants of an increase in their self-confidence.
I am happier with who I am because of the surgery and a lot more confident. (UM, two years post-LSG, female)
After the surgery when one loses so much weight, you can wear beautiful dresses again. How could anyone be unhappy? (PE, two years post-LSG, female)
5. Eating behaviour and relationship with food
Participants often reflected on changes in the ways that they interact with food since the surgery.
My brain says that I can only eat small amounts so I would rather go for something that I really, really love like [a] muffin rather than a sandwich, which I can only eat half of ... (BR, three years post-LSG, female)
The ability to be in control of portion sizes was mentioned as one of the key factors in their success.
I was brought up [thinking that] you eat everything on that plate or you don’t leave the table … But, if I look at a meal now and there is one mouthful left but because of the sleeve I do feel full, I just push it away. (NC, two years post-LSG, female)
Nevertheless, they frequently pointed out that the surgery was not a guaranteed way of changing their interaction with food, which still required significant effort (both mental and behavioural) on their part. They needed to change the way they thought about food, as well as changing their eating behaviours.
A lot of people think it is a cure, but it is not, it is a tool to help you lose weight. You still [have] to work hard if you still want the results. (JO, three years post-LSG, female)
6. Societal influences
The negative view that society has of obesity was often mentioned, and patients compared their perceptions of how they feel they are viewed since having the surgery with how they felt they were viewed prior to the surgery.
I felt very ostracised, so self-conscious being overweight. (BR, three years post-LSG, female)
If you had social things, you would try to make an excuse that you didn’t have to go … and I don’t really feel like that anymore. (MA, two years post-LSG, female)
Their belief that they were now more socially acceptable because of their weight loss was expressed in descriptions of expanded societal engagement.
I did go away with work for 10 months actually, and when I think about it I don’t know if I would have been as comfortable doing that prior to my weight loss. (CA, two years post-LSG, female)
I find that skinnier people are [now] quite friendly with me. (GE three years post-LSG, female)
7. Body image
While patients did mention negative aspects of their personal appearance when they were overweight (as already explored in ‘2. Physical changes and daily improvements’), they tended to focus more on the positive outcomes of their appearance since the surgery.
There was a significant focus from female participants on the ability to buy and wear clothing that they liked.
It’s lovely to walk into a shop and buy something I like rather than because it fits me. (NC, two years post-LSG, female)
Usually I’d have to buy something a little bit bigger because I know I’d put the weight on. I used to have to buy maternity clothes. (ST, one year post-LSG, female)
However, the struggle with excessive skin after weight loss was mentioned by a number of participants, with further surgery sometimes being required to deal with this.
I elected to have an abdominoplasty. I have had that done because I had the biggest apron that hung. You can say it’s vanity but it was awful and I was getting terrible fungal infections and I would have to pick it all up to dry underneath. I was putting baby cream around. (NC, two years post-LSG, female)
8. Relationships
Relationships within families were usually described as being enhanced after the surgery.
I used to get really tired and used to have naps whereas now I have much more energy, so also I don’t get angry at the kids; I’m a bit more tolerant. (HO, two years post-LSG, female)
However, many participants mentioned fear of or actual experience of judgement from friends regarding the surgery.
One of my best friends, who is actually a large lady, doesn’t talk to me anymore. (RO, three years post-LSG, female)
A number of participants were so concerned with being judged that they opted to only disclose the fact they were having surgery to a small group of people. They used the term ‘secret sleever’ to describe themselves, and explained that this is a term used in social media to identify patients who have undergone LSG ‘secretly’ (ie only disclosing to their most trusted family and friends).
[M]y husband, close girlfriend and a sister-in-law … are the only people that know I had [the surgery] ... [T]hat’s the only thing I suppose that I feel a little bit sad [about]. I haven’t been open or honest with people [because of] fear of judgment. (NC, two years post-LSG, female)
Discussion
Overall, the level of satisfaction following LSG was high in study participants. They described the weight loss as positively affecting their ability to participate in a wide range of activities including social interactions and exercise regimens. Furthermore, even the 25% of patients who reported side effects in the survey did not report low levels of satisfaction. This suggests that side effects are bearable when considering the magnitude of positive impacts on other aspects of their lives. This is in contrast to what health professionals may determine to be important following surgery.12
The concept of finding a ‘new normal’ after surgery was one of the overarching themes clearly communicated by participants. This was described as a difficult but generally worthwhile process; they were at pains to point out that the surgery was a tool and not a guarantee of success in achieving these changes in their lives.
Participants expressed the sense of control they now felt in a range of aspects of their lives, not simply over food, and this was something they felt was overall a positive change in their lives.
A sense of ambivalence was often present during the interviews, as participants expressed their satisfaction with the changes in their lives overall but a need to acknowledge that these had come at a cost. This is in line with a recent systematic review of the literature on all bariatric surgery (not only LSG), which found that for a considerable time post-surgery, patients continue to strive for control and normality in some aspects of their lives.13
An unexpected finding from both the survey and the interviews was the extent to which the LSG improved participants’ involvement in exercise. Prior to surgery, most had exercised to try to lose weight, but without success. Research into pre-operative attitudes towards exercise has found that many patients understand the important health benefits of exercise; however, they have a number of obesity-related barriers to participating in adequate levels (eg pain, physical limitations, concerns over their presentation).14 Patients also describe non–obesity related barriers to exercise including a lack of time and a lack of motivation.
The significant increase in motivation described by the participants post-surgery is encouraging. After the surgery, their exercise tolerance improved (75% stated a high to very high improvement in tolerance), and their enjoyment of exercise also increased. There was uptake of a range of different activities, with exercise no longer seen as something to be endured but rather something to be enjoyed. The benefits of exercise go significantly beyond weight loss,15 so it is encouraging to know that LSG results in most patients increasing their exercise frequency and tolerance.
Those patients who did not exercise post-operatively described physical (eg arthritis pain, fatigue) and social (eg time limitation) barriers. It is important to consider post-surgical stamina and chronic comorbid conditions when providing appropriate exercise prescriptions, and to help patients overcome time and motivation impediments to exercising.16 A change in perception of exercise from weight-based to health-based may also be a useful strategy, particularly for female bariatric patients.17
A further insight that was obtained from this project was that of the existence of ‘secret sleevers’. Several of the participants felt that surgery was misunderstood by many as being a ‘cheat’s way out’, and they felt they would be judged for having had it done. Therefore, they only told a select group of people about their surgery. They stated that this is a reasonably common decision made by patients, and there are hidden Facebook groups for ‘secret sleevers’ who wish to support each other privately.
Interestingly, there was no difference in both the qualitative and quantitative results across the time span since having the surgery. This means that effects experienced (both positive and negative) after one year appear to persist over time, with no new changes or considerations identified at the three-year mark.
Limitations
The study is limited in that it is a single-centre study with patients from one surgeon, and examines patient experiences up to just three years post-operatively. Although the participant rate of 22 interviewees was respectable when compared with other qualitative research in this field, the participants who responded were potentially those who felt that the surgery had been successful for them. However, it is also likely that those who had poor experiences also wanted the opportunity to tell their story. Future important research would be to deliberately seek perspectives of those who had neutral or unsuccessful results.
Conclusion
Overall, patients in this study were satisfied with choosing to undergo LSG surgery, up to three years post-operatively. In addition to the LSG procedure improving metabolic outcomes, there were impacts on broader physical and psychosocial aspects of their lives as they journeyed to find a ‘new normal’, gain control and wrestle with ambivalence. The positive effect that LSG has had on participants in a number of areas (eg improved exercise, more positive and controlled interaction with food, enriched social engagements and improved body image) must be balanced by the reports of the challenging nature of the full lifestyle change, the fear of weight regain and the perceived judgement they received from friends and society. These factors are all important considerations for both patients and healthcare providers to consider before and after undergoing LSG.
Implications for general practice
What the research adds to the literature
This research gives some patient-centred perspectives of life after LSG in the Australian setting, including the effect on patients’ exercise, eating habits and social interactions. Effects of the surgery go well beyond metabolic improvement and risk reduction, and psychosocial impacts (both positive and negative) are a significant component of the patient experience.
Implications for Australian general practice
Even though a patient may fit the NHMRC criteria for bariatric surgery and be able to access it through their private health cover, it is an elective surgery that needs to be carefully considered before a referral is made.
It is the authors’ hope that this research gives general practitioners and other healthcare providers a more nuanced understanding, with realistic expectations of what a patient’s life may look like after the surgery.
Finally, it should be emphasised that surgery is not an ‘easy cure’, but it can certainly be a helpful tool.