The term ‘athlete’ appears in more than 30,000 titles or abstracts among all PubMed-indexed articles, although it remains unclear where and when this term originated. When searching in the same database by ‘athlete definition’ or ‘definition of athlete’, not a single citation has been found.1 To have an unambiguous definition, Araujo et al have provided the following, which will be used within this article. To be an athlete, four criteria should be simultaneously fulfilled:
- to be training in sports aiming to improve his/her performance or results
- to be actively participating in sport competitions
- to be formally registered in a local, regional or national sport federation as a competitor
- to have sport training and competition as his/her major activity or focus of interest, almost always devoting several hours in all or most of the days to these sport activities, exceeding the time allocated to other professional or leisure activities.1
Challenges
Some of the more significant challenges facing both the primary care physician and athlete are being able to identify the risks to the athlete of sustaining a sudden cardiac arrest (SCA), recognising a sports-related concussion (SRC) and attempting to eliminate doping violation in sport. Additional challenges facing the older athlete have previously been addressed.2
Sudden cardiac arrest
Incidence
Sudden cardiac death (SCD) in sport has a likely incidence of 1:50,000 to 1:80,000 athletes per year.3 The incidence is higher in males and certain ethnic groups.4 SCD comprises 16% of all deaths of athletes, which is more than the percentage of deaths attributed to suicide, drug overdose and heat stroke combined.3 It has been estimated that the incidence of SCD in athletes is twice that of the general population.5
Obtaining accurate figures for SCD and SCA is difficult. Not all cases are reported, some are misclassified and many studies looking at the incidence had inclusion criteria so varied that it was difficult to accurately comment on significance; therefore, the true incidence may only be speculated and remains unclear.6 As a result of this categorical uncertainty, within this article, the terms SCA and SCD will be collectively referred to as SCA.
The distribution of cardiac disease and incidence is variable by country.7
Causes
Although the most common causes of SCA in athletes are somewhat speculative,6 it appears that some common causes within various age groups fit a pattern, as outlined in Table 1. This table should be viewed in the context of there being significant overlap in the conditions leading to SCA within the different age groups. In athletes aged <35 years, inherited and/or congenital heart disease are among the more common causes, whereas atherosclerotic coronary artery disease continues to have the highest incidence in athletes aged >35 years.8,9 In addition to age, other factors that contribute to SCA include sex, lifestyle, race and ethnicity.3–9 There are causes of SCA that are not particular to any age group; some of these are outlined in Table 2.
| Table 1. Potential causes of sudden cardiac arrest in the athlete by age |
| |
Age group |
| |
<16 years |
16–35 years |
>35 years |
| Condition |
Myocarditis |
Hypertrophic cardiomyopathy |
Ischaemic heart disease |
| Potential cause |
Often secondary to viral or bacterial infection |
Most often inherited |
Adverse lifestyle factors
Inherited risks |
| Potential outcome resulting in sudden cardiac arrest |
Arrhythmias, cardiac failure, cardiogenic shock
May result in dilated cardiomyopathy |
Ventricular arrhythmias |
Ventricular fibrillation
Pulseless ventricular tachycardia
Asystole |
| Electrocardiographic findings pre-event |
Sinus tachycardia
Non-specific ST segment and T wave changes |
T wave inversion and ST depression, usually in the infero-lateral leads, or prominent (wide) Q waves |
May be normal, or show ST and/or T wave changes |
| Potential symptoms pre-event |
Usually sub-clinical; shortness of breath and tachycardia may be present |
Most often asymptomatic unless severe
If severe:
- breathlessness
- chest pain
- rapid or irregular heartbeats
- light-headedness
- syncope
|
May be asymptomatic, or have:
- chest pain
- shortness of breath (especially on exertion)
- light-headedness
- palpitations
|
| Table 2. Potential causes of sudden cardiac arrest in all age groups |
| |
Condition |
| |
Commotio cordis |
Long QT syndrome |
Brugada syndrome |
Wolff–Parkinson–White syndrome |
| Potential cause |
Direct impact to chest overlying left ventricle (precordium) |
Dysfunction of ion channels located in cardiac cells (ion channelopathy) |
Dysfunction of ion channels located in cardiac cells (ion channelopathy) |
Accessory electrical pathway |
| Potential outcome resulting in sudden cardiac arrest |
Primary arrhythmic event (R-on-T phenomena)
Ventricular fibrillation after impact |
Lethal arrhythmia |
Lethal arrhythmia |
Lethal arrhythmia |
| Electrocardiographic findings pre-event |
Nil relevant prior to event |
May be normal
Male athletes
QTc ≥470 ms
Female athletes
QTc ≥480 ms |
Coved ST segment elevation >2 mm in >1 of V1–V3 followed by a negative T wave |
May be normal
Short PR interval
Wide QRS complex
Delta wave (slurring of the initial portion of QRS)
ST segment and
T wave discordance |
| Potential symptoms pre‑event |
Nil |
Majority asymptomatic |
Majority asymptomatic |
Related to tachycardia:
- palpitations
- shortness of breath
- light-headedness
- fainting
|
In primary care, there is a presumed high level of awareness regarding the prevention, detection and management of atherosclerotic coronary disease, with somewhat less awareness of the inherited and/or congenital heart diseases.
It is important to note that, with the exception of myocardial ischaemia and hypertrophic cardiomyopathy, chest pain is a rare feature of many of the cardiac conditions leading to SCA in young people. Subsequently, the absence of chest pain is not a reliable or valid rule-out criterion when assessing SCA risk.
Screening
The focused history is an essential component to support a correct diagnosis. Family history and any associated conditions such as diabetes and elevated body mass index always warrant further investigation.
Antecedent symptoms and family history may be absent in over 80% of cases of SCA,10 making screening somewhat difficult albeit essential.
Any symptoms of excessive breathlessness, light-headedness, chest pain, irregular heartbeat or syncope with physical activity are potential red flags that must never be ignored. No person experiencing these symptoms must ever be allowed to continue with physical activity without first receiving a thorough cardiac assessment and subsequent clearance to continue their activity.
A resting 12-lead electrocardiogram (ECG) is an essential baseline investigation for anyone in any age group with clinical suspicion and for all people over the age of 35 years involved or planning involvement in a physical activity. For elite and professional athletes of any age, a periodic resting 12-lead ECG is mandatory prior to competition in most sporting codes.
The majority of disorders associated with an increased risk of SCA are suggested or identified by abnormalities on a resting 12-lead ECG,11,12 most often identified with abnormalities of the ST and/or T waves. The fact that a normal athlete ECG can differ from a normal non-athlete ECG makes ECG interpretation more difficult. Figure 1 outlines normal and abnormal athlete ECG patterns, with Figure 2 showing some examples of classical ECG findings. Figure 3 shows an example of a normal non-athlete ECG. Figures 4–7 show some classical features of abnormal ECG patterns.
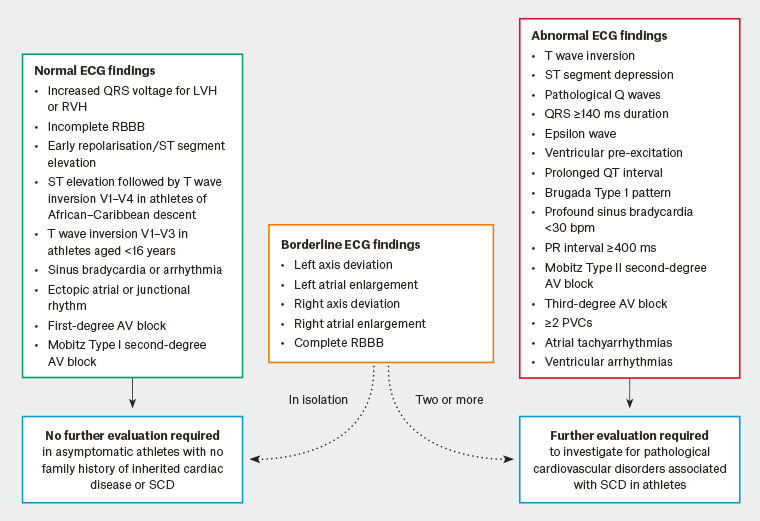
Figure 1. International consensus standards for electrocardiographic interpretation in athletes12,39
AV, atrioventriular block; bpm, beats per minute; ECG, electrocardiogram; LBBB, left bundle branch block; LVH, left ventricular hypertrophy; PVC, premature ventricular contraction; RBBB, right bundle branch block; RVH, right ventricular hypertrophy; SCD, sudden cardiac death
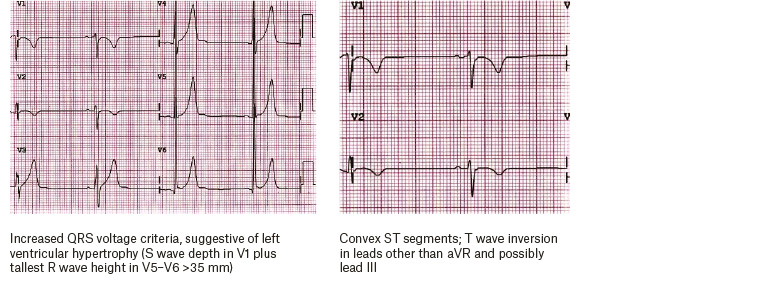
Figure 2. Typical electrocardiographic findings for the athlete
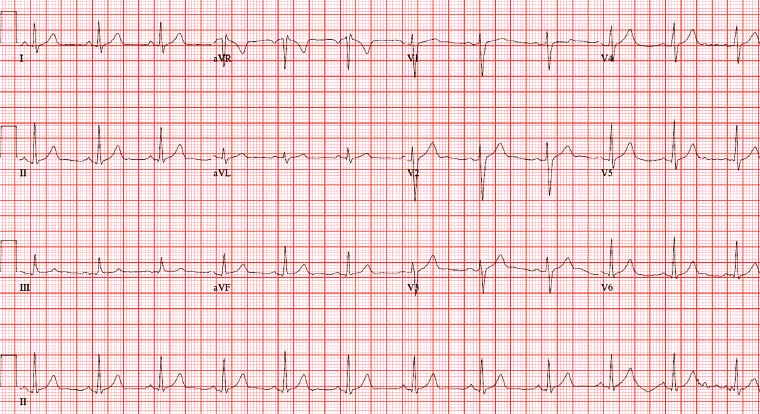
Figure 3. Example of a typical non-athlete electrocardiogram. Normal T is upright except aVR and possibly III; T should follow orientation of QRS; R wave should elongate from V1–V6; QRS predominantly negative in V1-positive in V6; QRS should be narrow (<3 small squares).
Any ECG that is identified as abnormal – particularly those that have ST or T wave abnormalities (such as in Figures 4–7) – should be considered suspicious. Referral for further interpretation and advice by a cardiologist experienced in the care of athletes is indicated. An echocardiogram should be considered as the next investigation to perform,13,14 and the patient should not be permitted to participate in physical activity until medically cleared.
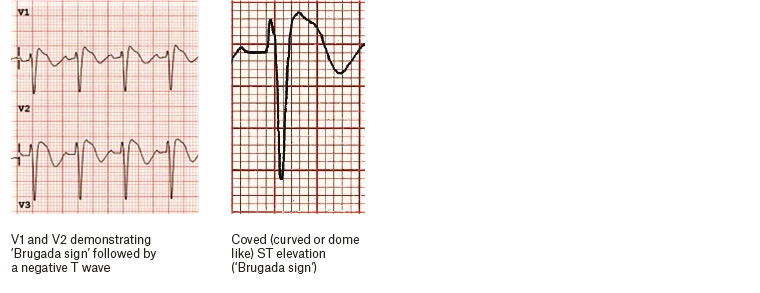
Figure 4. Electrocardiography findings for Brugada syndrome
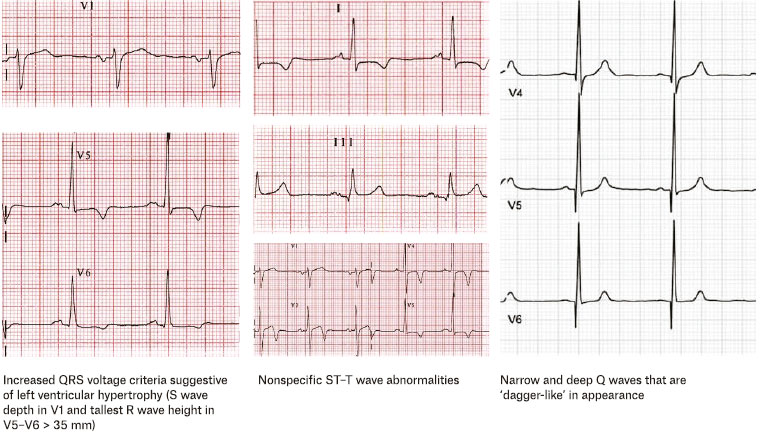
Figure 5. Some characteristic findings for hypertrophic cardiomyopathy on electrocardiography
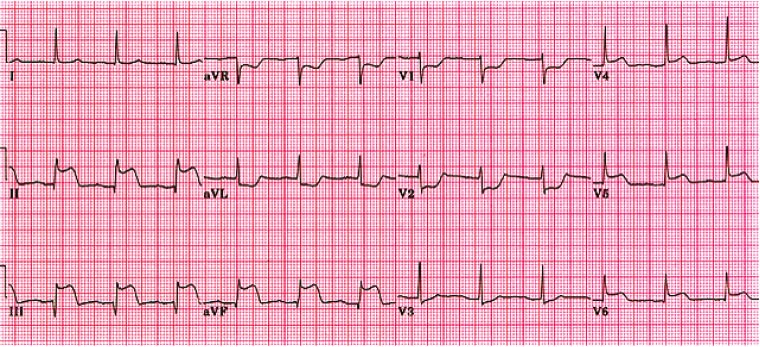
Figure 6. Example of electrocardiogram during an acute myocardial infarction, demonstrating ST segment elevation in leads II, III, aVF and V4–V6 with reciprocal ST changes in V1–V3
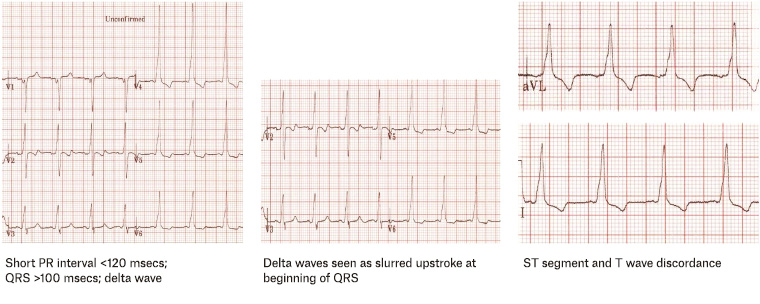
Figure 7. Possible electrocardiographic findings for Wolff–Parkinson–White syndrome
Management
During physical activity, syncope or vasovagal episodes should never be considered as benign events. Therefore, an athlete who sustains a sudden syncope and collapse without impact or contact with another player or object must always be considered to have sustained an SCA until proven otherwise. In this situation, immediate response, early cardiopulmonary resuscitation and defibrillation are the priorities. If defibrillation is not immediately available, effective cardiac compression is the first priority.15 In an SCA, for every one-minute delay in defibrillation, the chance of return of spontaneous circulation decreases by 10%.16,17
Sports-related concussion
Background
There is increasing attention, both through mainstream and social media as well as legal interest, on sports-related concussion (SRC). The primary care physician caring for concussed athletes has an ethical obligation to ensure that they safeguard the current and future physical and mental health of their patients.18
There is evidence showing the likely connection between repeated episodes of concussion and cognitive impairment, depression, suicide and chronic traumatic encephalopathy.18–22 Subsequently, SRC has become an area of significant concern and interest for athletes, sporting organisations, governments, the media and doctors.
The Consensus statement on concussion in sport has outlined the 11 ‘Rs’ of SRC management: Recognise, Remove, Re-evaluate, Rest, Rehabilitation, Refer, Recover, Return to sport/school, Reconsider, Residual effects and sequelae, and Risk reduction.23 Table 3 outlines these stages. The approach to concussion assessment and management should be no different for the athlete and non-athlete populations.
| Table 3. The 11 ‘Rs’ of sports-related concussion management23 |
| Stage |
Action |
| Recognise |
Direct or indirect force to head
Loss of consciousness not always a feature
Assess memory, Glasgow Coma Scale and cervical spine
Apply Sports Concussion Assessment Tool, version 5 (SCAT5) or Child SCAT5 |
| Remove |
If indicated by SCAT5 or Child SCAT5, immediately assess for red flags
If any uncertainty, always remove from play |
| Re-evaluate |
Focused history and examination
Determine the need for neuroimaging and neuropsychological assessment
Implement tools such as CogSport or CogState |
| Rest |
Absolute cognitive and physical rest for 24–48 hours following injury
Gradual and progressive reintroduction of physical and cognitive activities
Aim is to remain asymptomatic |
| Rehabilitation |
Focused on specific symptoms experienced
Multidisciplinary
Includes physical, cognitive, psychological, social and sporting needs of athlete |
| Refer |
Symptoms still present after two weeks in an adult and four weeks in a child
Multidisciplinary and experienced centre |
| Recovery |
Severity of symptoms in the acute phase is the strongest predictor of a slow recovery |
| Return to sport/school |
Stepwise program according to SCAT5 or Child SCAT5
Minimum of 24 hours in each step
Recurrence of symptoms mandates return to previous asymptomatic step |
| Reconsider |
Special considerations may apply to particular populations including children and adolescents |
| Residual effects/sequelae |
Increased risk of cognitive impairment, depression, suicide and chronic traumatic encephalopathy |
| Risk reduction |
Identify those with previous sports-related concussion and attempt to mitigate risks |
Definition
SRC is a traumatic brain injury induced by biomechanical forces. Subsequently, the impact received to the head may be direct or indirect, and loss of consciousness may or may not be a feature. There is typically short-lived and potentially subtle impairment of neurological function that resolves spontaneously, although both the timeline and symptoms are variable and individual. It is important to note that the majority of SRCs occur without loss of consciousness or frank neurological signs.23 Standard structural neuroimaging studies typically fail to identify any abnormality.
Diagnosis
Currently there is no gold standard diagnostic tool for SRC, although there are accepted sideline screening tests including the Sports Concussion Assessment Tool, version 5 (SCAT5)23,24 for players aged ≥13 years and the Child SCAT5 for players aged <13 years.23,25 More detailed tests of cognitive and neurological function include the Maddocks questions26 and the Standardised Assessment of Concussion;27 the SCAT5 is inclusive of both.
The SCAT5 and Child SCAT5 are designed only for use by doctors and licensed healthcare professionals, who must be familiar with both tools and how and when to apply and interpret them correctly.
In the sporting context, orientation questions involving time, place and person are unreliable26 and should not be used. Rapid sideline screening, rather than providing a definitive diagnosis, is the priority. The SCAT5 and Child SCAT5 are divided into on-field and off-field assessments, with the off-field assessment being more detailed.
In addition to the initial SCAT5 or Child SCAT5, further assessment must always be performed. The re-assessment process includes a thorough clinical reassessment, determination of the need for neuroimaging and neuropsychological assessment using web-based tools such as CogSport or CogState. There is also a stepwise strategy for return to sport and/or school, which is outlined in SCAT5 and Child SCAT5.
Management
If a player experiences tonic posturing, loss of consciousness or balance disturbances, or if there is any suspicion of SRC, the player must always be removed from play, immediate medical management implemented and a more detailed assessment undertaken using the subsequent sections of the SCAT5 or Child SCAT5.
Any player involved in a contact collapse who is unconscious or semi-lucid must be considered as having sustained a traumatic brain injury (TBI), spinal injury and potentially a compromised airway until proven otherwise and managed accordingly.
Following the diagnosis of an SRC, there should be a period of complete physical and cognitive rest for 24–48 hours. After this initial phase, the patient may be encouraged to become gradually and progressively more physically and/or cognitively active, although they must remain below the threshold that provokes symptoms. This threshold is very variable and individual.
Rehabilitation following an SRC is dependent on the symptoms experienced, the stage following the injury and the athlete’s individual demands. Rehabilitation should be multidisciplinary where possible, and consideration should be given to the physical, cognitive, psychological, social and individual needs of the athlete, as well as their sporting demands. Symptoms that are present after two weeks in an adult, and four weeks in a child, following an SRC mandate referral. If possible, the athlete should be referred to a collaborative multidisciplinary facility skilled in managing SRC in such cases.
When should the athlete return to sport?
Graduated return to sport, school and/or work is a stepwise rehabilitation strategy and is outlined in the SCAT523,24 and Child SCAT5.23,25 In general, each step of the strategy should take 24 hours to complete.
Progression through the stepwise program should therefore take a minimum of one week before return to usual activities. If concussion symptoms occur at any stage of the program, the athlete must step back to a stage at which they were completely symptom free and recommence progression from that stage.
Increased severity of the person’s symptoms in the first 24–72 hours following injury (the acute phase) are the strongest predictor of a slow recovery.23 Determining complete recovery is difficult, and it is likely that the physiological and psychological time to recovery is much longer than clinical recovery time. That being said, the athlete must not return to pre-injury cognitive and physical exertion until completely symptom-free.
There is a paucity of literature available about the child and adolescent athlete with SRC, with the most appropriate assessment, management and return-to-sport strategy for the child or adolescent athlete yet to be defined.25 Until these are defined, the SCAT5 and Child SCAT5 are the most appropriate screening tools currently available. It is expected that the duration of SRC symptoms is up to one month for the child and adolescent athlete.23
Doping
Doping in sport is a significant challenge for sporting and anti-doping authorities. It compromises the integrity of sport, increases the risk to personal safety and health for those who are doping, and has the potential to create an unfair advantage in training and competition.
Many adverse analytical findings in athletes are unintentional and the result of consumption of supplements containing banned substances of which the athlete is unaware. The majority of these tainted supplements are classified as nutritional supplements, muscle-bulking agents, weight-reduction agents or health foods. These classifications downplay the potential risks these supplements may hold.
In a recent meta-analysis, substances prohibited by the World Anti-Doping Agency (WADA) were found in most of the supplements analysed.28 The most frequently encountered components in these products were anabolic steroids.29 In all cases, these substances were not listed on the product information for the supplement.
Consumption of supplements often starts at a young age30 and is encouraged by parents, coaches and peers. This paves the way for ongoing abuse and has been described as the ‘gateway to doping’.31,32 Supplements that appear benign – such as vitamins, minerals, muscle-bulking agents and weight-loss products – are easily obtained either online or over the counter in supermarkets or pharmacies. The unregulated nature of online purchasing makes it particularly concerning.
Supplement use in athletes is likely to be higher than anticipated. Studies have suggested that the use of supplements in various sports ranges from 62%33 to 88%.34–37
Currently, in Australia, medicinal products such as herbs, vitamins, minerals, nutritional supplements, and homoeopathic and certain aromatherapy preparations are referred to as complementary medicines and are regulated as medicines under the Therapeutic Goods Act 1989 (www.legislation.gov.au/Series/C2004A03952). Some supplements may be classified as foods rather than medicines and therefore are categorised under the Australian and New Zealand Food Standards Code (www.foodstandards.gov.au/code/Pages/default.aspx), which is enforced by the states and territories and therefore has less strict regulation.
Although regulation is in place, currently this is only for products purchased within Australia. Australia uses a two-tiered system, with complementary medicines classified as ‘lower risk medicines’, which are not necessarily listed on the Australian Register of Therapeutic Goods (ARTG). Some complementary medicines are exempt from the requirement to be included on the ARTG.
With the current system in place and the ease of purchasing supplements over the internet, there is a significant risk of supplements containing banned substances.
Most athletes consume supplements without consulting a physician38 and are likely to be unaware of the potential risks associated with supplement use. Although abiding by the WADA regulations is mandated for all athletes and is ultimately the athlete’s responsibility, the physician should be aware of the likelihood that an athlete is taking supplements and the possibility of contamination with a banned substance.
The opportunity to educate the athlete about the health and doping risks associated with supplement use should be a priority for the physician. The WADA and Australian Sports Anti-Doping Authority websites provide valuable information and easy references for both the athlete and physician. Referral to an accredited sports dietitian is always appropriate when managing and educating athletes on performance, nutrition and supplementation.
Key points
- Anyone with any clinical suspicion and those aged >35 years involved or planning involvement in physical activity must, as a minimum, have a resting 12-lead ECG.
- Any ECG with ST and/or T wave changes not considered normal for the athlete or non-athlete must be considered as suspicious and referred for further investigation. The athlete must not participate in physical activity until medically cleared.
- Any athlete who is involved in a non-contact collapse and who is unconscious must be considered as having sustained an SCA until proven otherwise. Immediate priorities are cardiac compression and defibrillation.
- Unconsciousness is not necessarily a feature of SRC.
- People suspected of an SRC must always be removed from play and the SCAT5 or Child SCAT5 applied.
- Any athlete involved in a contact collapse who is unconsciousness or semi-lucid must be considered as having sustained a TBI, spinal injury and the potential for a compromised airway until proven otherwise. Immediate priorities are airway patency and spinal stabilisation.
- The majority of athletes take nutritional supplements without their doctor’s knowledge.
- Supplement use is the leading cause for doping violations in sport.
- Many supplements contain substances that are banned in sport and not listed on the product information.
- The potential health risks associated with supplement use are significant.
Resources