News
Aboriginal communities turn remoteness into an advantage
Grassroots efforts have so far proven successful in controlling the spread of coronavirus in remote communities.
 Congress Health Promotion staff who have been focusing on community education about COVID-19 and supporting Aboriginal people in Alice Springs who are in quarantine.
Congress Health Promotion staff who have been focusing on community education about COVID-19 and supporting Aboriginal people in Alice Springs who are in quarantine.
‘We’ve taken big steps to try and control the virus in this area, not just trying to flatten the curve. And it’s working so far.’
Dr Sam Heard, GP and Medical Director of the Central Australian Aboriginal Congress (CAAC) Aboriginal Corporation, is among the health workforce on the ground in Alice Springs.
He knows more than anyone that the prospect of coronavirus spreading among Aboriginal and Torres Strait Islander people is concerning, given the vulnerability of elders and the high prevalence of comorbidities that are present from a younger age. One in eight live in overcrowded housing, which could see the virus spread rapidly.
From the beginning of this crisis, community leaders and Aboriginal Medical Services (AMS) have stepped up and taken rapid action, advocating for stringent measures needed to protect their most vulnerable.
‘Everybody was immediately thinking about how to protect the population, not just individuals, but how to protect everyone we’re looking after and that extended into all the community in Central Australia really,’ Dr Heard told newsGP.
The CAAC was the first organisation to call for control zones in Central Australia in a bid to cut down movement in and out of Aboriginal communities.
Other significant initiatives have included those led by the Northern Land Council, the Anangu Pitjantjara Yankunytjatjara (APY) Lands, and the Torres Strait Islands and Papua New Guinea border cross regions, who have stopped issuing new permits for visitors. All non-urgent travel and visits by government and non-government agencies have also been cancelled.
‘That was all Aboriginal initiative,’ Dr Heard said.
‘Aboriginal people realised very early on their general populations living out bush were extremely high risk for this virus and turned remoteness into an advantage.’
Additional grassroots efforts also continue to ensure vital information around social distancing and hygiene is disseminated in a culturally appropriate way.
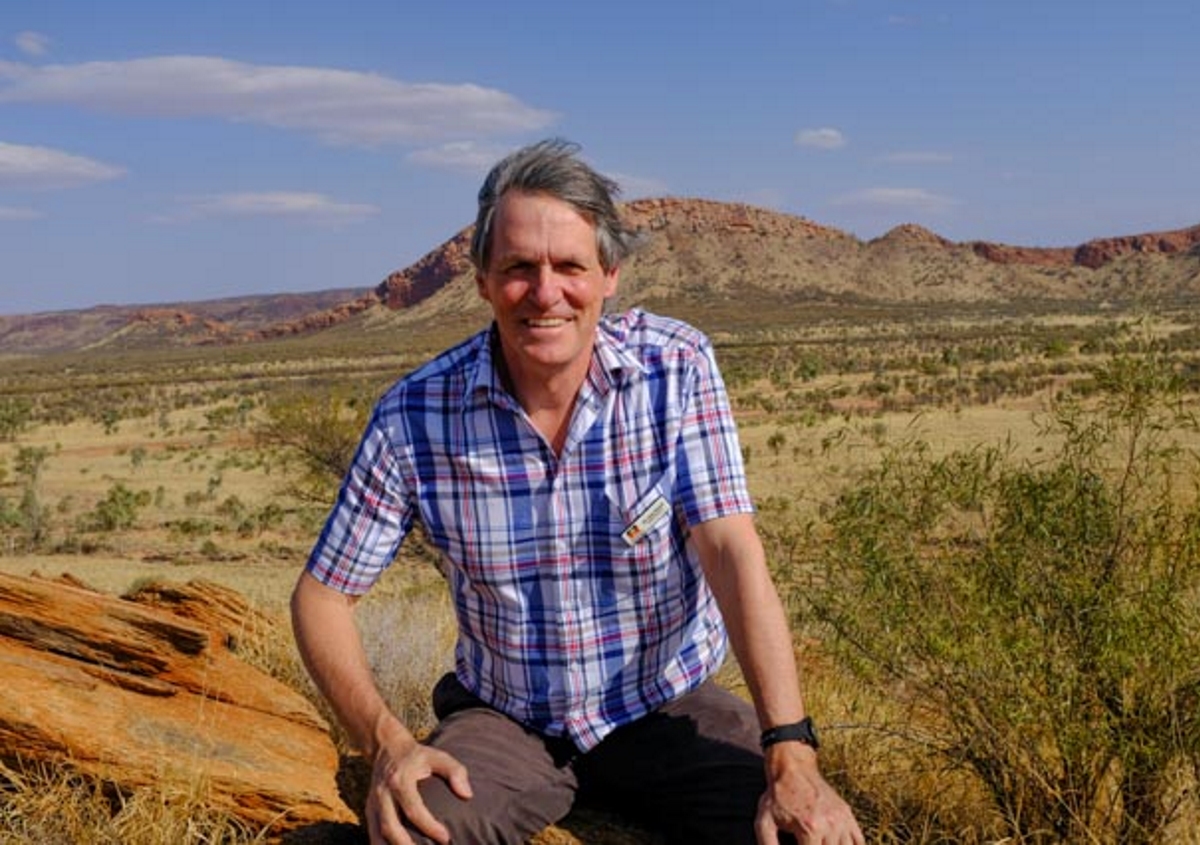
Dr Sam Heard is concerned at the prospect of coronavirus spreading among remote Aboriginal and Torres Strait Islander communities. Image: Flinders University
The Northern Land Council has produced informative videos in 18 different Aboriginal languages which will be distributed this week among communities across the state.
‘It’s a big message to get across, as it goes against the culture,’ Dr Heard said.
‘If you came and saw Aboriginal people who are out there educating people every day, just the energy they’re putting in and interest in helping people understand social distancing and what’s involved.
‘There aren’t a lot of words in Aboriginal language for pandemic and this sort of thing.
‘The AMS’s are really working hard in this area and it’s been successful so far. Whether it can remain this way, we’ll have to find out, but certainly we have a glimmer of hope that we might be able to actually control the disease in this area.’
Six new confirmed cases of coronavirus in the Kimberley, Western Australia, five of whom are health workers, has shown the dire need for these ongoing efforts.
The Northern Territory, at the time of publication, has 21 confirmed cases of coronavirus, 19 of whom are locals.
A border lockdown, in place since 31 March, requires anyone that enters the territory, other than essential workers, to quarantine for 14 days, while WA is set to implement a temporary near-total border closure from midnight on Sunday 5 April.
The Federal Government has allocated $123 million in funding over two years to support Aboriginal and Torres Strait Islander businesses and communities during the pandemic, including $10 million to expand the reach of night patrols to enforce social distancing and travel restrictions.
‘We will get through this together by everyone following the health advice and complying with the restrictions that are necessary to protect our elders and our culture,’ Indigenous Australians Minister Ken Wyatt said.
But Dr Heard admits that anxiety is high and that there are continued challenges.
The introduction of control zones has resulted in hundreds of people going remote, with 800 making the move in one day, Dr Heard said. This has placed a strain on community resources, with stores rapidly running out of goods.
Meanwhile quarantine measures, while necessary, have made it difficult to get health workers into place quickly.
‘One issue is that the APY Lands are actually in South Australia. They relate to us, so we’ve still got some work to do because that causes problems. If we’ve got a nurse in the Northern Territory that lives in Alice and works in the APY lands, they’ve got this quarantine barrier,’ Dr Heard said.
With a high dependence on short-term locums, it is near impossible to have someone in quarantine for two weeks and then working for a week – ‘It doesn’t work,’ he said.
While staffing is adequate at this stage in Alice Springs, in very remote areas Dr Heard admits they are struggling and says the pandemic is an opportunity for health workers, particularly doctors and nurses classed as vulnerable, to lend their services.
‘I would like to think that some people later in their careers might be interested in coming to help us at this point,’ Dr Heard said.
‘It’s a couple of months of living in a nice space, we’ve got training and it’s probably the safest place at the moment for older health practitioners to work because you’re not exposed to [the coronavirus].’
Log in below to join the conversation.
Aboriginal coronavirus COVID-19 cultural safety Torres Strait Islander
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?