News
AIHW report highlights ‘vast burden’ of chronic disease
Around one in two Australians over the age of 15 had a long-term health condition in 2019–20, a patient survey has revealed.
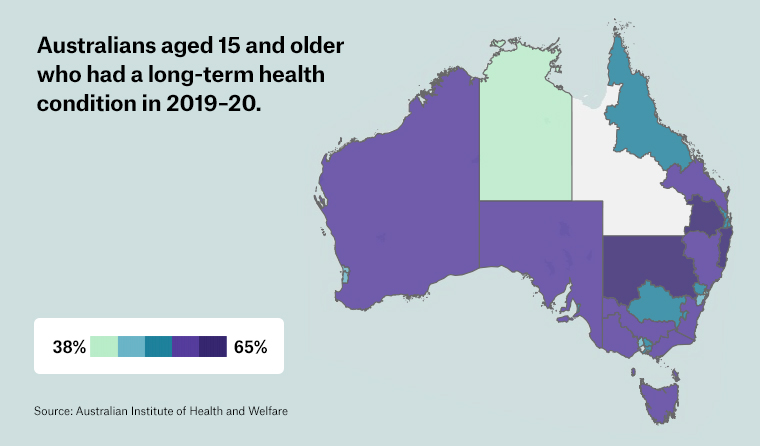 More than half the population over the age of 15 (51.6%) reported having a long-term health condition in 2019–20.
More than half the population over the age of 15 (51.6%) reported having a long-term health condition in 2019–20.
People within the North Sydney Primary Health Network (PHN) typically report being more healthy than in any other part of Australia, according to a newly released study from the Australian Institute of Health and Welfare (AIHW).
The survey, which compares patient experiences for 2019–20 across each of the country’s 31 PHNs, found 93.2% of patients in North Sydney say their health as excellent, very good or good – compared to the national average of 86.5% and Country South Australia, which stood at 81.2%.
Dr Edwin Kruys, Chair of the RACGP Data Governance Advisory Committee, says while it is challenging to comment on specific regions, the survey does contain both heartening results for general practice, as well as broad areas of concern.
In particular, he told newsGP the fact that more than half the population over the age of 15 (51.6%) reported a long-term health condition has implications for general practice and healthcare more widely.
‘Although we should probably be a bit careful with the interpretation, the data appears to highlight the vast burden of chronic disease,’ Dr Kruys said.
‘Countries that respond effectively to this global trend have been developing community-facing healthcare systems. Unfortunately, Australia still has a long way to go in this respect.’
There is also cause for concern surrounding the affordability of care, Dr Kruys said.
He highlighted the finding that 3.7% of adults delayed or did not see a GP due to worries about the cost, with the highest proportion of these found in Tasmania (8.6%). The survey also found 6.6% of adults had delayed or avoided filling a prescription for the same reason.
‘Most GPs know from experience that there is a growing group of people unable to afford healthcare,’ Dr Kruys said.
‘Average out-of-pocket costs have increased significantly over the past decade because of lagging patient Medicare rebates.
‘My concern here would be that this group is contributing to the unsustainable growth in demand on public hospitals, [by] receiving hospital care because of complications or exacerbations of chronic disease that could have been better managed in general practice.
‘When I was working in an urgent care hospital setting, patients regularly advised they were unable to afford general practice out-of-pocket costs and could not always get in to see their GP at short notice.’
On a more positive note, the vast majority of patients said they were satisfied with the way their GP interacted with them; 92.3% of patients across Australia felt their GP listened carefully to what they had to say, peaking at 96.3% in the Nepean Blue Mountains PHN.
The results were even higher when patients were asked if their GP always or often showed respect for what they had to say, with a national average of 94.6%.
‘This is in line with other surveys over the years, consistently demonstrating high patient satisfaction rates with general practice,’ said Dr Kruys. ‘Although expected, it is still a great result.’
However, a significant proportion of adults still felt they had to wait longer than acceptable to get a GP appointment, with 18.6% stating this as a concern in the survey.
Dr Kruys said he believes this should be explored further for the potential knock-on effects it could have on secondary and tertiary care.
‘Although these figures should be interpreted carefully – and by the way they are about the same for other specialists – it may indicate a potential general practice access problem due to various factors, most of which are out of the control of healthcare providers,’ he said.
‘GP practices usually have same-day appointments available for adults and children with urgent problems, but anecdotally the demand seems to be rising.
‘In my opinion there is enormous untapped potential for collaborative care models between state hospitals and general practice to facilitate care closer to home. These models could also support improved general practice access if and where needed.’
The AIHW report distils localised detail from the 2019–20 Patients Experience Survey carried out by the Australian Bureau of Statistics.
It was compiled from 29,793 respondents who contributed to the ABS’s Multipurpose Household Survey (MPHS) and published without any geographic information last November.
The survey suggested women were significantly more likely to see a GP (87.7% compared to 78.6%), while the likelihood of a GP visit increased among older patients, with over-85s at 98.3% compared to 70.9% for those aged 15–24.
It also found that more people in the North Coast of New South Wales had a preferred GP than in any other part Australia – with notable differences across the country.
The 86% of patients with a preferred GP in the North Coast PHN in NSW is far higher than the around two-thirds of adult residents within the Country Western Australia PHN, which has one of the lowest rates in Australia.
Results for the Northern Territory were lower still, but the statistics come with a cautionary caveat that they exclude the Indigenous Community Strata, which comprises an estimated 25% of the population in the territory.
Log in below to join the conversation.
AIHW chronic disease general practice Primary Health Networks
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?