News
Alert issued over antibiotic-resistant gastro
Doctors have called the drug-resistant infections a reminder about the public health threat posed by antimicrobial resistance.
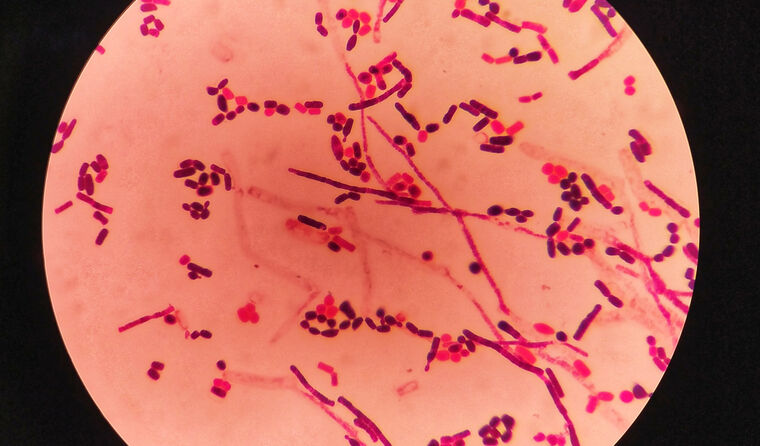 Multidrug-resistant shigella strains are circulating among the Victorian community.
Multidrug-resistant shigella strains are circulating among the Victorian community.
On 11 July, outgoing Victorian Chief Health Officer Professor Brett Sutton issued an alert for growing cases of antibiotic resistance detected in shigellosis intestinal infections, caused by the shigella bacteria.
In Victoria, two or more related cases is considered indicative of an outbreak and require investigation, according to the state’s health department, which is carrying out contact tracing for the spread of infections, mainly reported among men who have had recent sexual contact with other men and returned overseas travellers.
Of particular concern is the bacteria’s increased resistance to antibiotics, with Professor Sutton warning that such infections ‘are a serious public health problem’ as they are harder to treat.
RACGP Victoria Co-Deputy Chair, Dr Aadhil Aziz, told newsGP the health alert is a reminder of the global public health threat posed by antimicrobial resistance.
‘We don’t have an unlimited supply of antibiotic groups, we only have a few different groups, and once we go through all of those groups, we’re in big trouble as humanity,’ he said.
‘There haven’t been new antibiotics developed for years, and even the newest ones that have been are ridiculously expensive.’
It is estimated that more than 1.27 million people already die each year from drug-resistant infection and Dr Aziz is worried that controversial pharmacy prescribing trials being undertaken across Australia, which have been widely opposed by the RACGP, will exacerbate the issue.
‘It’s very simple – if we’re overusing or unnecessarily or inappropriately using antibiotics for coughs, colds and such, or just randomly giving antibiotics out when somebody says, “I think my pee is burning”, that could be really detrimental in the long run,’ he said.
‘It’s like shooting ourselves in the foot because these antibiotics protect us when we really need them, [for example] with serious brain infections like meningitis.
‘If we use antibiotics incorrectly then our bodies change them and they mutate, then they become resistant, and most often nowadays we are getting multidrug-resistant bacteria.’
For Victorian GPs, Dr Aziz echoes the department’s advice to remain aware of the symptoms of shigellosis, and that antibiotic treatment should be reserved for cases of ‘severe infection’ or those who are immunocompromised.
‘We need to make sure that the other doctors in the area are more aware of it, so that if a patient is to present with diarrhoea [for example], it can be front and centre and – depending on how long the symptoms drag on for … decide whether to send the stool culture, then we can diagnose shigella,’ he said.
‘[While] most of these conditions are self-limiting, there are a few that need to be treated with antibiotics and that’s only if the patient is not getting better or has other comorbidities.’
The highly contagious shigellosis bug is mostly spread via the faecal and oral routes, with hallmark symptoms including acute onset of diarrhoea, fever, nausea, vomiting and abdominal cramps.
Symptoms usually develop 1–3 days following exposure, but in some cases can occur from 12 hours to one week afterwards.
Dr Aziz said GPs should apply their same leadership approach from the COVID pandemic response.
‘We are always concerned and/or aware, but we’re not the type of profession that panic, we’re usually pretty level-headed,’ he said.
‘And we will face it calmly as what we did with COVID, and as that progressed and changed, we changed our management and strategies to evolve with COVID, and it’s the same thing for something like this.
‘As long as we continue to give patient education, get the news out on how to limit the spread and … look after your immune system … I don’t think we’ll have anything that’s going to be uncontrollable.’
The Victorian Department of Health issued the following advice for clinicians:
- Request a stool culture when investigating for shigellosis
- Antibiotic treatment should be reserved for cases of severe infection or those who are immunocompromised
- Antibiotic choice should be based on susceptibilities and advice should be sought from an infectious disease specialist or microbiologist, as antibiotic resistance varies by region and over time
- Patients should be advised to maintain good hygiene and safer sex practices, avoid preparing food for others and be excluded from work if they are a priority case until cleared by their Local Public Health Unit
- Clinicians and pathology services must notify the Department of Health of any cases of shigellosis within five days of diagnosis
- Local Public Health Units are following up people diagnosed with antibiotic-resistant shigella infections and their contacts to provide advice about symptom monitoring, testing and exclusion requirements
Log in below to join the conversation.
antibiotic resistance infectious disease shigellosis Victoria
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?