News
Are infections and antimicrobial resistance linked to pandemic deaths?
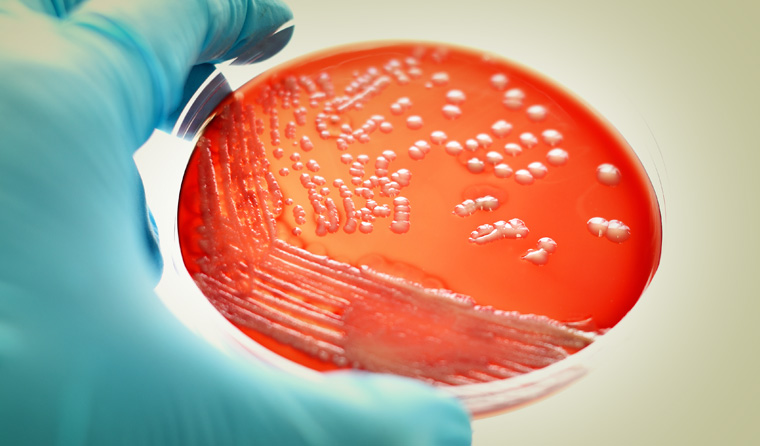
Secondary bacterial infections are emerging as a risk-multiplier for coronavirus patients – with drug-resistant infections a particular threat.
 Are antibiotic-resistant secondary infections linked to pandemic death rates? Some experts say it’s more than likely.
Are antibiotic-resistant secondary infections linked to pandemic death rates? Some experts say it’s more than likely.
During the 1918 Spanish Flu pandemic, many people succumbed not to the influenza virus, but to secondary pneumonia, as opportunistic bacteria took advantage of a weakened immune system and invaded the lungs.
An influential 2008 Journal of Infectious Diseases study – co-authored by leading US infectious disease expert Dr Anthony Fauci – found most Spanish Flu deaths were in fact due to bacterial pneumonia.
These infections were hard to treat, given the virulent strain of flu emerged a decade before the first antibiotic, penicillin, was discovered.
‘If the next pandemic is caused by a human-adapted virus similar to those recognized since 1918, we believe the infection is likely to behave as it has in past pandemics, precipitating severe disease associated with prevalent colonizing bacteria,’ the study authors conclude.
Now this prediction looks to be coming true. Experts are warning that history may be repeating a century later during a new pandemic, with secondary bacterial infections emerging as an understudied way people can die from COVID-19.
We have antibiotics this time – but overuse of the vital drugs has led to the emergence of strains of antibiotic-resistant organisms.
Not only that, the current global pandemic may supercharge the growth of antibiotic-resistant organisms, given many hospitalised coronavirus patients are routinely given antibiotics to reduce the risk to healthcare workers.
‘The COVID-19 pandemic has led to huge numbers of people with compromised immune systems being admitted to hospitals, which are a known breeding ground for drug-resistant bacteria. Because of this influx, these hospital-associated bacteria will now have a much wider potential target group,’ microbiologist Dr Ronel McCarthy notes in The Conversation.
Infectious disease expert and ANU microbiologist Peter Collignon told newsGP it is doubly concerning given that increasing antimicrobial resistance may make these infections harder to treat.
‘During the Spanish Flu, between half and three quarters of the deaths were linked to secondary bacterial infections. In a study from Wuhan, half the [COVID-19] patients who died had a secondary bacterial infection. That’s quite high,’ he said.
The Wuhan study in The Lancet was small, involving 191 patients who already had advanced COVID-19, leading antibiotic resistance research network ReAct to caution that the secondary infections were very late stage, with sepsis and acute heart and kidney injuries having occurred in many patients, and to call for more research.
Professor Collignon predicted that mortality rates will be worse in nations with higher rates of antimicrobial resistance, such as China, Italy and India.
‘Where is the worst antibiotic resistance in Europe? Italy and Spain. The death rates there are considerably higher,’ he said.
‘There’s a much higher chance that if you get a secondary bacterial infection it won’t respond to antibiotics,’ he said.
‘I have a view that antibiotic resistance is important in this pandemic. It makes sense. If you go into an ICU [for any reason], a proportion get secondary bacterial infections.’
India had the highest rate of resistance of 41 nations in a 2018 BMJ study, while China’s gram-negative bacterial resistance is ‘severe’, according to a 2019 Frontiers in Microbiology study.
India’s National Centre for Disease Control has called on state health authorities to ensure hospitals adopt strict infection prevention guidelines to stop transmission of both coronavirus and bacterial infections.
An anonymous national health official told Indian newspaper Mint that the move was to stem the impact of antimicrobial resistance.
‘[Antimicrobial resistance] can indirectly impact the outcomes of treatment in COVID-19 patients. We have asked all the hospitals to adopt the guidelines while treating coronavirus patients,’ the official said.
Almost all COVID-19 cases in India ‘conclude in serious pneumonia’, Dr K Madan Gopal of India’s NITI Aayog thinktank told Mint.
‘Now, if this secondary infection is triggered by antibiotic-resistant bacteria then the situation becomes grave and harder to treat.’
Adding to the issue is the fact hospitalised coronavirus patients in some countries have been given antibiotics without a confirmed infection in order to reduce the risk to doctors from aerosol-generating diagnostic procedures, according to Wired reports.
Microbiologist Dr Adam Roberts and collaborators have collated emerging research on secondary infections and antibiotic use, such as a Lancet study flagging increasing concern that COVID-19 patients are at risk of contracting a dangerous fungal infection, invasive pulmonary aspergillosis.
Virologist Jeffery Taubenberger, who first sequenced the genome of the Spanish Flu, has told Bloomberg that secondary bacterial infections in the lungs can prevent patients from recovering due to the damage they can do to respiratory tract stem cells.
‘[Without these cells] you just can’t physically repair your lungs’ he said.
People who have a mild reaction to the coronavirus tend to be those able to contain it to the upper respiratory tract. Worse trajectories occur if the virus is able to move to the lungs, potentially paving the way for a secondary assault by bacteria, according to Dr Taubenberger, who was a co-author of the 2008 Spanish Flu study.
Paul Glasziou, Professor of Evidence-Based Practice at Bond University, told newsGP it is likely that countries with high numbers of COVID-19 cases will also have increased rates of antimicrobial resistance.
‘A lot of the seriously ill cases get secondary infections. If you have higher rates of antimicrobial resistance, you’re going to have more deaths because you won’t be able to treat the secondary infections,’ he said.
But Professor Glasziou said antimicrobial resistance could actually decrease in nations like Australia, where the infection has been broadly contained, given that many people have been avoiding GPs and hospitals – thus reducing the number of antibiotics prescribed.
‘You have an increased use of antibiotics for hospitalised COVID-19 cases but, at the same time, you’ve got a reduction in ambulatory care visits with the number of people seeing GPs down and elective surgery put off or cancelled,’ he said.
Social distancing and handwashing have also slashed rates of influenza and other respiratory infections.
‘As well as stopping coronavirus, these interventions also stop every other acute respiratory infection – and that’s the major area of [antibiotic] overuse in primary care,’ Professor Glasziou said.
‘What it means long term is hard to say; it depends on what behaviours are changed by this.
‘We may have changed some behaviours permanently and that could lead to long-term reductions in acute respiratory infections. And that could help us long term with antimicrobial resistance.
‘That’s my hope – I’ve got my fingers crossed. It will be interesting to look at.’
Log in below to join the conversation.
antimicrobial resistance coronavirus COVID-19
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?