News
Are vaccines alone enough to avoid COVID mortality?
The emergence of highly infectious variants could see the risk of death remain at high levels, according to new modelling that has been described by some as ‘pessimistic’.
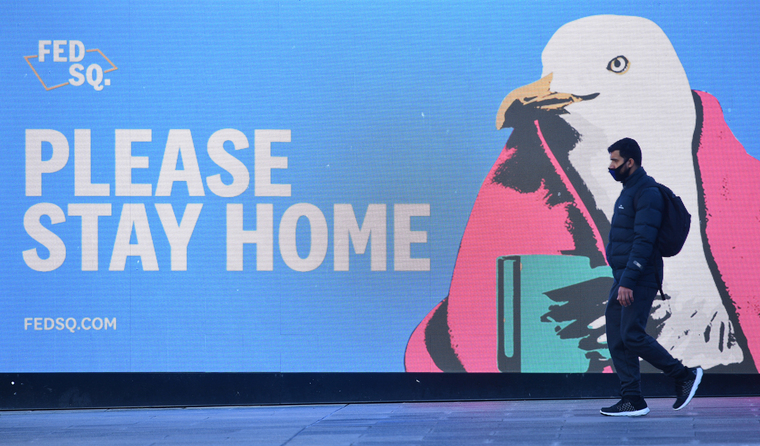 Experts say that public health measures will need to remain a key line of defence against COVID-19 for the foreseeable future. (Image: AAP)
Experts say that public health measures will need to remain a key line of defence against COVID-19 for the foreseeable future. (Image: AAP)
Millions of Australians have been able to breathe a sigh of relief while rolling up their sleeves to receive their COVID vaccine. It is a moment that seemed out of reach more than 16 months ago when SARS-CoV-2 first started making global headlines.
But even with moderate-to-high vaccine uptake, new modelling by the Burnet Institute suggests vaccine hesitancy and the emergence of new variants with the potential for reduced efficacy could still result in thousands of COVID deaths in Australia.
However, that’s not to say they are inevitable.
Rather, Burnet Institute Deputy Director and leading infectious diseases and public health specialist, Professor Margaret Hellard says the modelling highlights the importance of lockdowns and other public health measures.
‘The model is suggesting that unless you have intermittently imposed some form of restrictions, then you would have deaths,’ she told newsGP.
‘So there needs to be a conversation about that and an awareness that even with a high level of vaccination, depending on the variants and depending on vaccine efficacy – things that we can’t necessarily predict – it may mean that we need to have ongoing, intermittent restrictions.
‘Now what they are, and the extent of them, may not be the same as the kind of lockdowns [we have had]. But if we want to avoid significant morbidity and mortality associated with COVID over the next coming years, we need to be mindful that vaccines alone will not necessarily get us there.’
Professor Hellard says the modelling highlights four key policy areas that need to be addressed now, so that Australia is not caught unprepared:
- the need for high levels of vaccination
- the, likely, ongoing need for some level of public health restrictions
- careful thought and planning around how Australia will open its borders, including the need for purpose-built quarantine facilities
- the need for Australia to engage globally, ensuring regional neighbours are also supported to get vaccinations.
‘It’s basically saying we need to have a conversation at a variety of levels as we go forward,’ she said.
‘COVID is not going to suddenly go away just because we have a level of vaccination at one particular point in time.’
The model is designed so that parameters around vaccine efficacy, viral infectiousness, vaccine coverage and the speed of the vaccine rollout can be modified.
One scenario put forwards assumes a COVID variant that is 1.5 times as infectious as the one that caused Victoria’s 2020 outbreak, and where 80% of people aged over 60 and 70% of younger cohorts have been vaccinated with a vaccine that is 50% effective at preventing infections and has 93% efficacy at preventing deaths.
In this scenario, if the virus enters the community when there is 60% vaccine coverage and there were no public health measures in place, 4885 deaths could take place in Victoria alone within 12 months.
If vaccine coverage were to increase to 95%, the number of deaths reduces to 1346.
Increase vaccine efficacy in this same scenario to 75%, and the modelling suggests the number of deaths after 12 months could be less than 1000.
The scenario assumes a vaccine rollout of 150,000 or 250,000 doses per week, and that on detection of the first case testing increases, positive cases are isolated, and contact tracing continues for up to 250 diagnoses per day. It also assumes that masks are recommended but not mandatory.
However, the modelling has been
called out by some experts as being too pessimistic, given it presents worst-case scenarios, and that it is unlikely public health experts would leave an outbreak unattended.
Professor Tony Blakely, an epidemiologist and public health medicine specialist, told
The Guardian that even though modelling is needed to examine what measures might be needed once international borders reopen, it is difficult because the situation keeps changing.
‘For example, the Burnet modelling is on one hand too optimistic, as variants such as the Delta variant are actually more infectious than their modelling allowed for, and on the other hand is probably a bit pessimistic, as we have learned the vaccine is probably a bit better at preventing transmission of Covid than they allowed for,’ he said.
‘However, what they are trying to do is important as it shows how essential vaccination is, and the message from the Institute that we require higher vaccine coverage and that Australia is unlikely to ever achieve herd immunity are smack on the money.’
New research shows that both vaccines currently in circulation in Australia are effective against Delta, a variant of concern, with two doses of the Pfizer vaccine 96% effective against hospitalisation, and AstraZeneca 92% effective.
Professor Hellard admits that ‘there’s no such thing as a perfect model’, but maintains that many unknowns remain around how COVID will evolve, which is why the model has been specifically designed to give people the chance to explore various scenarios.
‘When people say this model is too negative or too positive, actually no, you’ve got the choice,’ she said.
‘They can go in and have a play with the Excel spreadsheet. You can put in different levels of vaccine uptake, you can put in level different levels of the virus infectiousness, you can put in different levels of vaccine efficacy into this model, which is on the website – you choose.
‘We actually don’t know what level of vaccination is required for “herd immunity” because we have changing variants, meaning you’ve got changing infectiousness of the virus, plus we have with that varying in the efficacy of the vaccine to the virus.
‘So I actually think that we have to be really careful about … [predicting] a specific level where we’ve reached “herd immunity”.’
While vaccine hesitancy remains a concern – a
survey conducted in June found 29% of Australians are either unwilling or don’t know whether they want to be vaccinated – Professor Hellard says it is vital to first ensure there are systems in place for effective uptake.
‘We have to stop going “the problem lies with them”,’ she said.
‘Rather than just simply talking about people not wanting to get a vaccine, say actually “how do we make it easy for people to get vaccinated? What are the structures in our systems?”
‘Because you can campaign all you like to tell somebody to go out and get vaccinated, but if they’re not in a position to stand in a queue for three hours, then that’s a really unhelpful vaccine campaign.
‘It’s not one size fits all, and it’s not set and forget.’
Log in below to join the conversation.
COVID-19 lockdowns masks modelling public health measures social distancing vaccine rollout variants
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?