News
‘Assume it’s everywhere’: aerosol fears underpin fight against COVID healthcare infections
Healthcare must learn from high staff infection rates and get ‘pandemic fit’ in case of a third wave, an expert says.
 Potential airborne spread underpins many of the Victorian Healthcare Infection Prevention and Wellbeing Taskforce’s recent safety decisions.
Potential airborne spread underpins many of the Victorian Healthcare Infection Prevention and Wellbeing Taskforce’s recent safety decisions.
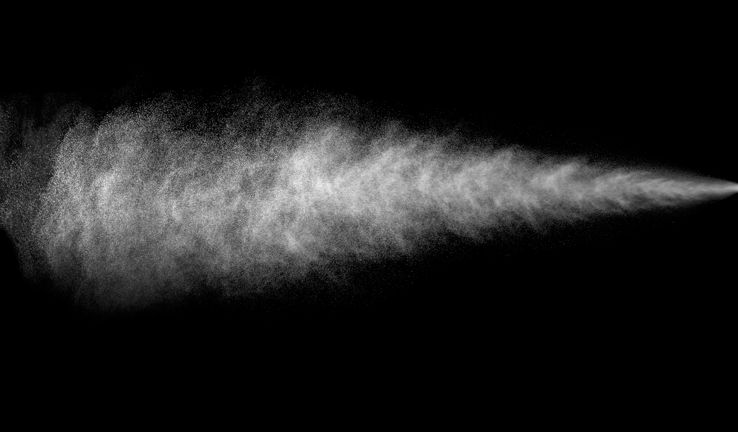
The likely aerosol spread of coronavirus underpins the precautionary approach taken by the new Victorian Government healthcare worker infection taskforce, according to a member.
Questions over how easily the SARS-CoV-2 virus is spread by small aerosolised particles lie behind recent charged high-level disputes between experts – and shape national guidelines on how best to prevent its spread.
But the Victorian Healthcare Infection Prevention and Wellbeing Taskforce is not waiting for a definitive answer, and is taking a precautionary approach in assuming the virus can be spread in aerosols, according to taskforce member Associate Professor Jane Munro.
‘Many of the initiatives coming from the taskforce target aerosol spread. Our slant has to be that COVID is aerosol spread, assume it’s everywhere and take the precautionary principle to protect healthcare workers,’ she told newsGP.
‘I’d perhaps want to be more forceful about [publicly talking about aerosol spread], especially to make sure every service is right onto changing their buildings or environments where necessary and to further educate healthcare workers about it.’
Mitigating the potential aerosol spread of coronavirus underpins Government efforts aimed at preventing any reoccurrence of the major transmission amongst staff at hospitals and aged care facilities, Associate Professor Munro said. This includes the Respiratory Protection program, which is introducing N95 respirator fit-testing across all Victorian healthcare services throughout September and October.
The taskforce was set up to address the spiralling infection rate among Victorian healthcare workers, who at one point accounted for two thirds of all new cases in a single day.
More than 3500 healthcare workers – primarily hospital nurses and aged care workers – contracted the potentially deadly virus during Victoria’s second wave.
Healthcare worker infections have fallen alongside the overall drop in community spread in Victoria, but still accounted for the majority of remaining new cases in recent weeks.
‘The fact we have had over 3500 healthcare workers infected in Victoria is not OK. It is not OK,’ Associate Professor Munro said.
‘The rest of Australia should also be on notice to make sure they are working to get all these systems prepared and people trained. This could happen anywhere with the right set up and load of COVID if the systems are not right.
‘This is not just about fit-testing. Are all the systems safe at work in office spaces? On wards and where you write up? In outpatients? In change rooms? Where people have a break or eat? Is ventilation up to scratch in older hospitals?’
To date, the taskforce has focused on providing guidance about changing hospital environments to better protect against the threat of infection.
These measures include removing chairs in break rooms to discourage sitting too close, closing eating spaces, increased training in workplace interactions, personal protective equipment (PPE) spotters, and the introduction of the Victorian Respiratory Protection program, which includes fit-testing.
The taskforce is also examining eyewear recommendations, general wellbeing, ventilation, and the environmental aspects of hospitals.
‘It’s about making sure healthcare workers are super-aware of personal protection, how to protect yourself, your mates, your team, [and] about being [as] aware as possible of the space you’re in,’ Associate Professor Munro said.
‘It’s also about the hospital being really aware of those spaces from an occupational health and safety point of view. Lots of hospitals have started going back and double-checking OHS [occupational health and safety] issues as much as possible to pull any occupational environment levers they can.’
Associate Professor Munro said tackling infections at work is about more than just better PPE.
‘This is about driving system change,’ she said. ‘It is not one single thing – it is about multiple levers.’
Healthcare worker advocate Associate Professor Alicia Dennis has called for more attention on what she calls ‘significant unresolved issues’ around infection rates in healthcare, specifically the need for official acknowledgement of airborne spread, higher levels of PPE, and data transparency.
However, the question of whether aerosolised small particles are a major cause of SARS-CoV-2 spread remains highly charged.
The US Centers for Disease Control and Prevention (CDC)
triggered the latest controversy by publishing new guidance suggesting it as a key way in which the virus could spread, only to quickly remove the information and claim it was an error.
Hundreds of scientists wrote an
open letter to the World Health Organization in July, calling for aerosol spread to be recognised as a major factor. Meanwhile, Japan
has acted as if aerosol-spread is a major vector for infection for months, leading authorities to focus on ventilation in indoor spaces and the need for fresh airflow.
In Australia, a
debate has raged between experts from the Federal Government’s Infection Control Expert Group (ICEG), which argues aerosol spread is real but not the major vector, and healthcare worker advocates and OHS experts who advocate taking the precautionary principle and acting as if aerosol spread is a real risk.
As recently as last month, ICEG Chair Professor Lyn Gilbert
told newsGP that ‘strong epidemiological and clinical evidence’ indicates that the predominant mode of transmission of COVID-19 is via direct transmission of droplets and/or contamination from surfaces and fomites contaminated by these droplets landing on them.
However, Federal Health Minister Greg Hunt later announced
a new partnership between ICEG and the National COVID-19 Evidence Taskforce in order to ‘review the latest evidence on infection prevention and control during COVID-19’.
‘The partnership will contribute to national infection control guidance by providing consensus guidelines on specific infection control issues that have emerged during COVID-19,’ Minister Hunt said.
Preparing for a potential third wave
Associate Professor Munro said it is very likely Australia will see a third wave before the pandemic is finally brought under control.
‘We have to get pandemic fit for the third wave, fourth wave, fifth wave, as the expert advice is that it is likely there may be future waves,’ she said.
‘Right now we can take the tiniest of breaths, with case numbers down in the community, then work like absolute demons to make sure all our systems are in place.
‘We have got to make sure we prepare in this phase now. We’ve done incredibly well compared to the rest of the world, other than Asia. So perspective is important, and learning from other countries and our colleagues where they have done well is really important.
‘But we’ve got to use this time going into summer cleverly and thoughtfully to get the healthcare system ready, to train our healthcare workers so we know what to do and [that] we’re ready for further outbreaks.’
According to Associate Professor Munro, better utilising GPs and community health will be crucial.
‘We need our contact tracing system as sorted as possible because that is the foundation piece of our COVID response,’ she said.
‘We need the healthcare system ready to protect healthcare workers, and we need aged care to be protected and ready.
‘We were not pandemic fit. Not just Victoria, the whole of Australia. This could happen in NSW in an instant. Their aged care is very [much] like ours.’
Associate Professor Munro said the Victorian Department of Health and Human Services has been ‘incredible’ to work with.
‘The taskforce has gone from 21 to 58 people in three weeks and is doing a mountain of work across all different aspects of healthcare worker infection and prevention,’ she said.
‘The department has been incredibly responsive. That was one thing I was worried about – but they really are listening.’
Dean of Health Sciences at Swinburne University Professor Bruce Thompson told
newsGP the issue that caught many health services off guard with COVID was the need to focus on the broader environment, rather than just the adequacy of PPE.
‘It was a broader issue of occupational health and safety. You could take a PPE approach – but there were so many [other] areas, from education to ventilation, to the size of rooms and corridors, to PPE spotters,’ he said.
‘If you took out “COVID” and put in “asbestos”, we would know what to do – appropriate PPE, how you take it off, negative ventilation rooms. In this case, we got caught napping.
‘Around 40% of transmission for healthcare workers was between each other. Environment and occupational health and safety should be above the individual level and that’s what needs a laser focus. If we have a third wave, we have to learn from this.’
Professor Thompson said the health system was not as prepared as it could have been to fend off infections amongst staff.
‘We were caught, and we can’t be caught again,’ he said.
‘Overall we did reasonably well, and compared to America we have done very well. But we can’t just forget what happened and go back to normal. That just can’t happen. There needs to be a step change.’
Associate Professor Munro is open to any feedback or ideas around preventing healthcare worker infections or improving wellbeing: Jane.munro@rch.org.au
Log in below to join the conversation.
COVID-19 healthcare worker PPE
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?