News
Claims GPs clogging up EDs ‘couldn’t be further from the truth’
GPs are calling for clearer guidance and adequate supply of PPE, amid concerns clinics are turning away infants with respiratory symptoms.
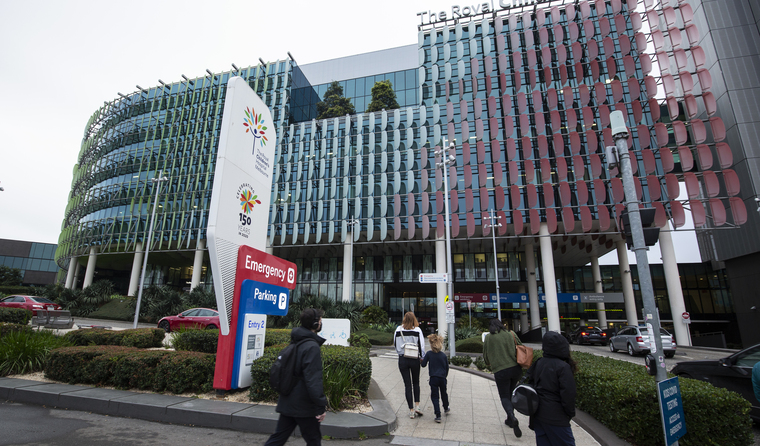 For some children with respiratory symptoms, RACGP Victoria Chair Dr Anita Muñoz believes the ED may be the most appropriate setting. (Image: AAP)
For some children with respiratory symptoms, RACGP Victoria Chair Dr Anita Muñoz believes the ED may be the most appropriate setting. (Image: AAP)
Victorian GPs who are reportedly refusing to see infants with respiratory symptoms have come under fire yet again, amid mounting concerns it is putting pressure on hospital emergency departments (EDs).
It comes just months after GPs pushed back on a letter issued by Queensland’s Chief Health Officer Dr Jeannette Young, which urged doctors to see patients face-to-face, claiming a third of ED visits could have been treated in general practice.
But RACGP Victoria Chair Dr Anita Muñoz says the college has been working alongside the Australian College of Medicine (ACEM), and that the reality on the ground suggests otherwise.
‘ACEM’s very clear on saying that this is a systems issue, not a GP issue,’ she told newsGP.
‘What we know from the data from ACEM, is that many of patients who are attending emergency departments that are category four and five are self-referred, so it’s got nothing to do with interaction with a GP.
‘And the majority of those that are self-referred, genuinely believe they have an emergency and genuinely believe the ED is the right place for them.’
However, for some children with respiratory symptoms, Dr Muñoz believes the ED may be the most appropriate setting.
She says there has been a push during the pandemic for children with symptoms to have swabs conducted by paediatric services, and that a cohort of children have been developing more severe respiratory illness due to a lack of exposure to viral fragments during lockdowns.
‘When things like RSV and rhinovirus re-circulated, a lot of the children had more severe versions of those illnesses than we are used to,’ Dr Muñoz said.
‘So those children were appropriately going to EDs.’
Looking back over the past 16 months, Dr Muñoz says it is clear doctors are willing to take whatever steps they can to cater to their patients, but that further support is needed to ensure everyone’s safety.
‘[Assessments] for those respiratory illnesses need to be done in a COVID-safe environment,’ she said.
‘And those COVID-safe environments at the moment are the GP respiratory clinics and health service environments that are designed to manage respiratory illness [and] aerosol generating procedures, and have negative ventilation and appropriate PPE.
‘Unfortunately, general practice has not been supported to create that environment.’
RACGP Victoria Deputy Chair Dr Bernard Shiu agrees and says reports of GPs turning patients away are contrary to doctors’ continued efforts to make use of telehealth, see patients in clinic car parks, and see patients face-to-face with ‘extremely limited’ PPE.
However, he believes some GPs simply do not have the capacity.
‘There are GPs that cannot see them for various reasons that are also appropriate … because they have no facilities or the GPs themselves are at risk,’ Dr Shiu said.
‘So those clinics will have to rely on either other clinics, or they will have no choice [but] to send patients to ED or a respiratory clinic to have the patients assessed.
‘Most of us actually are still seeing patients in some shape or form. But we have to follow the Chief Medical Officer’s advice on who to see and how to see them, and what is required before we see them, including getting the COVID-19 test, getting our staff to have PPE, and also seeing them in an appropriate manner.’
The latest PPE guidelines, published by the Infection Control Expert Group (ICEG) last week, state that if there is direct patient care for individuals with suspected or confirmed COVID-19 that P2/N95 respirators should be worn instead of a surgical mask.
But inadequate access to PPE is an ongoing issue that has made it difficult for GPs to cater to all patients, Dr Shiu says.
‘If they want us to [do this], then yep fine, but you have to help us protect our staff,’ he said.
‘The new guidelines from them for tier 1 and tier 2 has to match with supplies; you can’t just put guidelines out when you don’t give us the supplies.
‘And then the fit testing as well has to be provided by the Government.’
RACGP President Dr Karen Price says that along with PPE, health authorities need to provide clear guidance on how to balance the risks and the needs of sick patients.
‘We need to understand from our public health leaders what exactly they expect us to do in this situation,’ she told the ABC.
‘We don’t want to be involved in something that’s against public health advice.’
Coming off the back of the state’s fourth lockdown, Dr Muñoz says GPs are feeling the very real risk that COVID poses to practices and vulnerable patients.
‘We’ve had three general practices in the last month have had to stand down an entire practice for two weeks because of COVID positive cases within the practice,’ she said.
‘An entire practice, all of its clinical staff, all of its services and all of those hundreds of appointments, while there’s a deep clean and the quarantine is undertaken, which I think is a disproportionate risk for general practice to be taking.
‘There’s this call for general practice to be part of our public health system, but [receive] none of the support public health services get in terms of funding those services.
‘These are the complexities of the conversation, which are being completely missed in the media about general practices being responsible for clogging up emergency departments.
‘That statement couldn’t be further from the truth.’
Log in below to join the conversation.
child health COVID-19 ED emergency department PPE respiratory symptoms
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?