News
Vaccine policy identifies priority groups – but order proves ‘contentious’
Healthcare workers will be among the first in Australia to receive any COVID vaccine, but it is not clear if they should be given access ahead of vulnerable groups.
 Prime Minister Scott Morrison urged anyone with concerns about the new vaccines to speak with their GP. (Image: AAP)
Prime Minister Scott Morrison urged anyone with concerns about the new vaccines to speak with their GP. (Image: AAP)
People at increased risk of exposure to coronavirus and those who work in settings with a high transmission risk are likely receive first access to a coronavirus vaccine when it becomes available, according to a new Australian COVID-19 vaccination policy endorsed by the National Cabinet.
The Federal Government expects the initial supply of any vaccines to be limited, and as a result three ‘priority groups’ of those most in need have been identified; however, determining which groups gain first access has been ‘difficult and contentious’.
Speaking after the National Cabinet meeting on Friday 13 November, Acting Chief Medical Officer Professor Paul Kelly told reporters the characteristics of any successful vaccine candidate will help determine which of the priority groups is at the head of the queue.
‘Will they protect against transmission or severe disease or both? That will be the fundamental driver of the prioritisation of the vaccine to various parts of the population,’ he said.
‘Those that are caring for vulnerable people, vulnerable people themselves, and those at highest risk of transmission will be at the highest priority.’
The first group includes healthcare workers, aged care staff, and disability support and quarantine workers.
Those at an increased risk of developing severe disease or having worse health outcomes – including Aboriginal and Torres Strait Islander people, older people, and those with underlying health conditions – constitute the second group.
Essential services workers from ‘key occupations’ that cover services ‘critical to societal functioning’ form the last group.
Professor Kelly also confirmed that new coronavirus vaccines will be provided free of charge to all Australians and Medicare-eligible visa holders.
Earlier in the day, Federal Health Minister Greg Hunt said he expects every Australian who wants a vaccine to have received one by the end of 2021.
Minister Hunt made the comments while touring the laboratories of the University of Queensland, which developed the molecular clamp vaccine of which the Federal Government has agreed to purchase 51 million vials should it prove safe and effective.
The company manufacturing the vaccine, CSL, is in the process of seeking regulatory approvals to begin phase 3 clinical trials before the end of 2020.
‘The initial data is very clear, that the vaccine is proving to be safe through phase 1 clinical trials and it’s proving to produce a positive antibody response,’ Minister Hunt said.
‘It is doing its job. That is particularly so in the elderly, and that is an especially important outcome, given the global vulnerability to elderly around the world from COVID-19.
‘It means that this vaccine will potentially be available, subject to the results of those trials, for delivery to Australians early in the third quarter of 2021.’
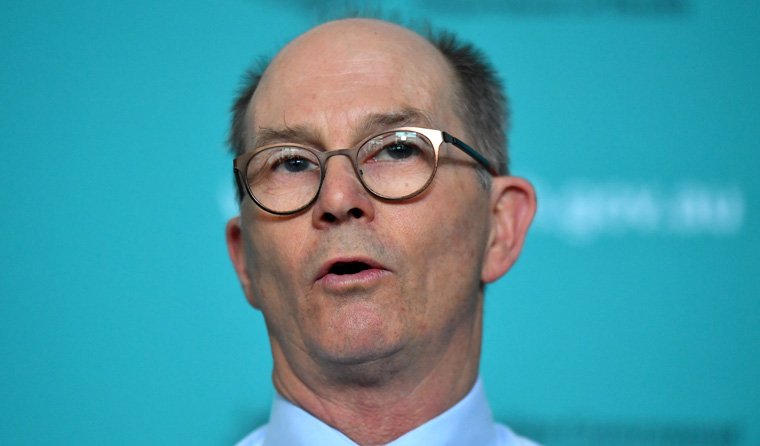
Acting Chief Medical Officer Professor Paul Kelly confirmed coronavirus vaccines will be provided free of charge to all Australians and Medicare-eligible visa holders. (Image: AAP)
Even though Minister Hunt would like to see every Australian vaccinated by the end of next year, it will not be mandatory. Regardless, Professor Kelly said he has no doubt the vast majority of Australians will volunteer to be immunised.
‘We are an excellent immunisation nation,’ he said.
‘Most people agree with immunisation being an important component of our preventative strategy for ensuring the health of the nation. We roll out new immunisation programs often.
‘I would say this has particular challenges as to the newness of it and so forth. And so we’re very aware that there will be people that are not wanting to have this vaccination or to spread information which is not true.’
Prime Minister Scott Morrison urged the public to be wary of misleading vaccine information circulating online, and directed anyone with concerns to speak with their GP.
‘There is a lot of misinformation that’s out there. You don’t go to Dr Google, you go to the doctor when it comes to these things and seek medical advice from your GP,’ he said.
‘There are no short cuts here. There are no lower benchmarks that apply to this vaccine.
‘It’s a very important vaccine for the country and for everybody’s health, but we will be applying the legal requirements that are there for people’s protection.’
Aside from providing information on priority access to the vaccine, Professor Kelly revealed that states and territories will be ‘very engaged’ in its distribution, and that the Federal Department of Health will establish a new in-house vaccine division.
While the first rollout of the country’s COVID-19 vaccinations program will not fall under the national immunisation program, the policy identifies general practices and GP respiratory clinics as two of the main vaccination locations, along with dedicated vaccination centres and temporary workplace clinics.
‘In-reach teams’ are likely to visit aged care homes and other vulnerable populations that may not be able to access other vaccination locations, and pharmacies have also been floated as a potential distribution point – depending on the safety profile of the vaccine.
Another outcome to emerge from the meeting is that NSW, Victoria and the ACT will participate in a contact-tracing pilot program that involves sharing information via a ‘light touch’ digital system.
This follows a recommendation from Australia’s Chief Scientist Dr Alan Finkel that all states and territories adopt a digital system to swap contact-tracing information quickly and efficiently.
Such a system has been deemed critical to the successful relaxing of state borders, all of which are slated to open by Christmas, with the possible exception of Western Australia.
‘As we go to a more mobile society, and a fully active economy, [states and territories] need to be confident that they can share information about people who are travelling from jurisdiction to jurisdiction,’ Dr Finkel said.
‘Now, at the moment the problem is not manifest. We don’t have a serious issue, but we need to be preparing.
‘We’ve recommended a very light-touch digital exchange mechanism that will respect all of the legislative and privacy requirements to enable states and territories to talk, to swap contact tracing information with each other, and access contact-tracing information from government agency databases.’
Log in below to join the conversation.
coronavirus COVID-19 immunisation vaccine
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?