Feature
Environment, not lack of willpower, responsible for obesity, expert says
Dr Georgia Rigas, Chair of the RACGP Specific Interests Obesity Management network, has urged media organisations to stop depicting people with obesity in a stigmatising and derogatory manner.
 Dr Georgia Rigas believes the media lacks images depicting people with obesity in a respectful and positive light. (Image: World Obesity Image Bank)
Dr Georgia Rigas believes the media lacks images depicting people with obesity in a respectful and positive light. (Image: World Obesity Image Bank)
Individuals with obesity are usually shown in the media as being lazy people who make poor lifestyle choices and who lack initiative to improve their health, according to an obesity expert.
Dr Georgia Rigas, Chair of the RACGP Specific Interests Obesity Management network, told newsGP that such images are offensive and only serve to further add shame, stigma and discrimination to individuals with obesity.
‘Too often … whenever there is an image [of a person] who is above a healthy weight, we see the cliché image of someone wearing a tight t-shirt, their stomach is overhanging, sitting on a couch …with a bowl of chips in one hand and a remote control in the other,’ Dr Rigas said.
‘So [if you] read between the lines, such negative images are reinforcing the perceived stereotype that people with obesity just sit on their bottoms all day, eating chips and watching TV.
‘Having managed patients with obesity for over a decade, I can assure you that this is not the case and that many people above a healthy weight are making healthy lifestyle choices, meal prepping, are physically active.’
Dr Rigas said the person’s head is usually also cut off in such images, making it less personable.
‘Whenever there are images depicting individuals with other health conditions such as diabetes or cancer, you see the whole person,’ she said. ‘Why isn’t this happening in images depicting individuals with obesity?
‘I urge everyone, in particular the media, to do away with such clichés and stereotypes.’
Dr Rigas said the language used to describe people with obesity is also usually disrespectful.
‘This has negative consequences on the physical, emotional and general wellbeing of individuals living with obesity,’ she said.
‘We need to change the dialogue and this starts with using people-first language.
‘As GPs we don’t treat “cancer patients”, we treat “people with cancer”. We should confer the same level of respect when talking to and managing people with overweight or obesity.’
Dr Rigas said there is a lot of misinformation suggesting that obesity ‘is a lifestyle choice and people choose to have obesity’, but the medical literature indicates the opposite is true.
‘I can assure you, having worked with individuals with obesity for so many years, that no one chooses to have obesity. If anything, they wish they didn’t have this illness so they wouldn’t be subjected to fat shaming, weight bias and weight discrimination,’ she said.
‘Obesity is a chronic progressive health condition with anticipated periods of relapse and remission.’
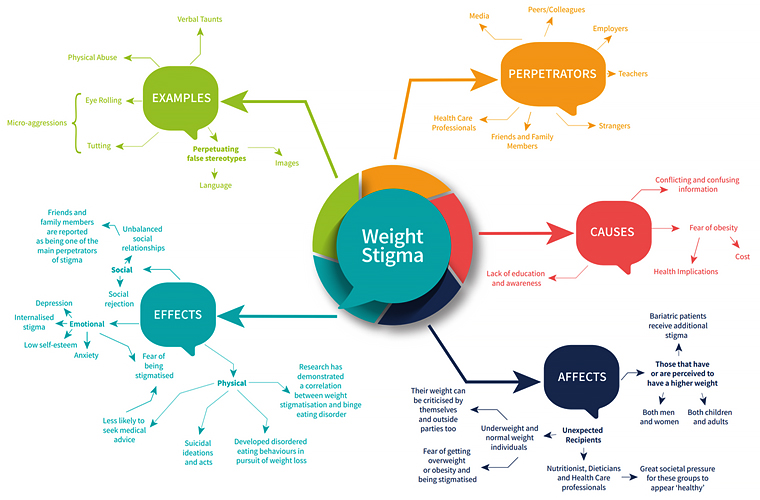 Weight stigma is a complex issue, with a wide range of drivers, sources effects and recipients. (Graphic: World Obesity Day)
Weight stigma is a complex issue, with a wide range of drivers, sources effects and recipients. (Graphic: World Obesity Day)
According to Dr Rigas, science indicates that the body physiologically defends against weight loss.
‘A person with obesity who has lost weight and is trying to keep it off struggles because they are essentially fighting their biology,’ she said.
‘The body’s hormones are trying to get them back to the weight they were before they lost weight.’
Energy expenditure, including desire to eat and exercise and, hence, weight management, is regulated by the hypothalamus, a part of the brain that is not under voluntary control.
‘However, this does not absolve individuals of their role to play or their responsibility in making healthier food choices, being as physically active as the body allows, and participating in mindful – rather than mindless – eating,’ Dr Rigas said.
Dr Rigas said society’s obesogenic environment is one of many contributors to those genetically predisposed to obesity developing the illness. Others include sleep deprivation, stress and changes in gut microbiota.
‘To quote American obesity researcher Dr George Bray, “Our genes loaded the gun, and the environment pulled the trigger”,’ Dr Rigas said.
She said weight stigma can be a double-edged sword, as people with obesity are less likely to seek medical help for their condition because they feel they will be judged.
‘Many studies show that people with obesity have concurrent depression or anxiety, reduced self-esteem, reduced work opportunities,’ Dr Rigas said.
‘Children who are above a healthy weight are more likely to drop out of school at an early age, and when they enter the workforce they usually have lower-paid jobs.
‘To add further salt to the wound, children and teenagers above a healthy weight are likely to develop obesity in adulthood and report fewer opportunities for job advancement.’
Dr Rigas said this all adds up to a continuing cycle, and is very distressing for individuals who are going through the journey.
‘There is also the issue of inequitable access to healthcare treatment in Australia, which I personally view as a form of discrimination,’ she said.
‘I can’t think of any other chronic health condition currently affecting more than six million Australian adults for which there is no anti-obesity medication on the [Pharmaceutical Benefits Scheme], and less than 1% of individuals potentially eligible for bariatric metabolic surgery are accessing such effective evidence-based therapy.’
obesity person-first world obesity day
newsGP weekly poll
Would it affect your prescribing if proven obesity management medications were added to the PBS?