News
‘Quite incredible’: Australia’s first monkeypox case spotted by GP
Health professionals should be vigilant, officials say, after the first likely cases of the virus were found in this country.
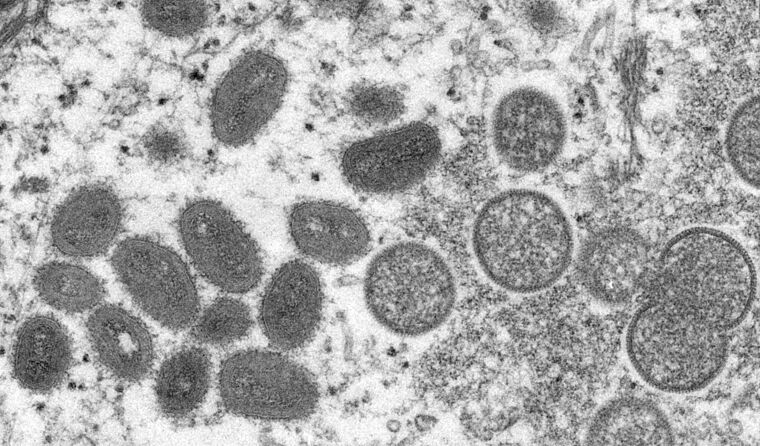 Electron microscopic image of a monkeypox virion. (Image: US CDC)
Electron microscopic image of a monkeypox virion. (Image: US CDC)
The identification of monkeypox, a rare smallpox-like illness, in several different countries over the past few weeks has attracted a large amount of attention.
On Friday, health authorities said the first likely cases had been discovered in Australia, including one in NSW and one in Victoria.
The first probable case was reported in Sydney in a man in his 40s who had recently returned from Europe. According to NSW Health, it was a GP who identified symptoms that appeared to correlate with the disease and arranged for urgent testing to be carried out.
The man reportedly developed a mild illness several days after returning to Sydney from overseas travel and presented to his GP.
The health authority said that confirmation testing was under way on Friday while the man and a household contact remained in isolation at home with the support of their GP and NSW Health.
The NSW Health Minister Brad Hazzard paid tribute to the GP involved.
‘I am always stunned at what our GPs and our medical practitioners can do,’ he said. ‘But since we’ve never seen it in this country before, it is quite incredible that a GP managed to identify this illness.
‘To have the capacity and skill sets to identify something that hasn’t been seen in New South Wales before is quite incredible and thank you to all of the GPs for all of the work that they do.’
The Victorian Department of Health later confirmed a case of monkeypox in the state, discovered in a man in his 30s who had recently come back from the UK.
It follows a number of cases overseas, including in the UK, Portugal, Spain, the US, Sweden, Belgium, Canada and Italy.
The disease is a zoonotic virus that can pass between animals and humans, as well as between humans, but is not considered easily transmissible without close contact.
According to the European Centre for Disease Prevention and Control (ECDC), it is the first time the disease has been discovered in Europe ‘without known epidemiological links to West and Central Africa’. Local transmission is strongly suspected.
The ECDC also states that the European cases include the first reported among men who have sex with men (MSM).
That was confirmed by NSW Chief Health Officer Dr Kerry Chant.
‘We're particularly urging men who are gay, bisexual or men who have sex with men to be aware of any unusual rashes or lesions and to contact by phone the sexual health clinic or GP without delay if they have any concerns,’ she said.
‘It is important to be particularly vigilant if you’ve returned ... from a large parties or sex on premises venues overseas.’
The first case was confirmed on 7 May by the UK Health Security Agency (UKHSA), which said that while the risk to the population remains low, it is urgently working to find how the cases were acquired.
Associate Professor Ian Mackay, a virologist from the University of Queensland, told newsGP that it is a case of being alert but not alarmed.
‘Local jurisdictions will have public health laboratories with testing capability, so it comes down to being vigilant for cases that meet the relevant clinical criteria,’ he said.
Symptoms of the virus can include:
- fever, chills, muscle aches, backache, swollen lymph nodes, and exhaustion
- an unusual rash, which typically starts on the face, then may spread elsewhere on the body.
The ECDC said recently detected cases have included ‘a preponderance of lesions in the genital area’.
‘The rash goes through different stages, and can look like chickenpox or syphilis, before finally forming a scab, which later falls off,’ an ECDC release stated.
‘The difference in appearance from chickenpox or syphilis is the uniform evolution of the lesions. The incubation period is typically 6–16 days but can be up to 21.’
The virus has two different strains, a Central African one and a West African clade.
The ECDC says the virus is usually mild with most people recovering within weeks, although it states that the death rate is higher among children and young adults as well as the immunocompromised.
‘The West African clade, which has so far been detected in the cases reported in Europe, has been observed to have a case fatality rate of 3.6% in studies conducted in African countries,’ the ECDC said in a statement this week.
On Thursday, the Department of Health in Victoria
also issued an advisory to health professionals about the disease.
According to
the Nigeria Centre for Disease Control, monkeypox was isolated and named in Copenhagen’s State Serum Institute laboratory in 1958 and was first identified in humans in 1970 in the Democratic Republic of Congo.
While endemic to Central and West Africa, the disease has previously been found in other parts of the world, mostly among returned travellers. The first known case on a different continent was recorded in the US in 2003.
The World Health Organization (WHO) states that vaccines used in the eradication of smallpox also offer some protection against monkeypox, while more recent vaccines have been specifically designed for the prevention of monkeypox but are not widely available.
The
estimated efficacy rate of the original smallpox vaccine against monkeypox is around 85%, according to the WHO.
The smallpox vaccine has not been used for decades since the eradication of the illness but
according to HealthDirect, vaccines have been stockpiled in Australia.
Marion Koopmans, Professor of Public Health Virology at Erasmus University Medical Center in the Netherlands said more information about the current disease is urgently needed.
‘The outbreak of monkeypox is starting to be worrisome,’
she said on social media this week.
‘We have seen occasional imported cases, usually dead ending. In this situation, new cases have been detected in different countries. That is very unusual.
‘Monkeypox as we know it is not that contagious. [The] question therefore is: was anything special happening explaining this situation? A very unusual index with many direct contacts for instance? Or is there something unusual about the virus?’
Professor David Tscharke, Head of the Department of Immunology and Infectious Diseases at the John Curtin School of Medical Research, Australian National University, also said the same vaccine used for smallpox could be effective for monkeypox even after exposure to the virus.
‘This is now being done in a process referred to as “ring” vaccination, where contacts are identified and vaccinated,’ he said.
‘The current epidemiology of monkeypox cases is unusual, because most cases are unlinked and will mean that vigilance is required across the world, but unlike SARS-CoV-2 this virus is better understood and methods to prevent spread can be actioned swiftly.’
Log in below to join the conversation.
infectious disease monkeypox smallpox vaccination
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?