News
GP’s AstraZeneca ‘matrix’ designed to help determine when to administer the vaccine
A Victorian GP has created a tool he believes will help to simplify the decision-making process for under-40s.
 Multiple changes in ATAGI advice have clouded the decision-making process for many people considering the AstraZeneca vaccine. (Image: AAP)
Multiple changes in ATAGI advice have clouded the decision-making process for many people considering the AstraZeneca vaccine. (Image: AAP)
Disclaimer: The tool discussed in this article is the sole creation of Dr Bernard Shiu and is not an RACGP-endorsed resource. GPs should make their own informed decisions about COVID vaccines, in consideration of ATAGI recommendations, when discussing them with their patients.
Dr Bernard Shiu, a practice owner in Geelong, has formulated the ‘matrix’ (shown below) to help in the decision-making process when younger patients enquire about the oft-maligned AstraZeneca vaccine.
Dr Shiu decided to define his own approach and make it publicly available after seeing so many questions on guidance in recent weeks.
His decision follows widespread confusion over administering the vaccine to age groups outside of the over-60s for whom it is the preferred option as outlined by the Australian Technical Advisory Group on Immunisation (ATAGI).
Dr Shiu feels the use of the word ‘preferred’ in the ATAGI advice implies younger people have more vaccination options than they currently do.
‘[The under-40s] don’t have a choice at the moment,’ he told newsGP. ‘Your choice at the moment is either AstraZeneca or wait. That’s the real choice.
‘I tested [the matrix] on a few patients and they all loved it.’
Dr Shiu said the reaction has been positive when he posted it on wider professional forums, with a number of fellow GPs requesting permission to use it in their own general practices.
‘The majority of them are absolutely loving it,’ he said. ‘The point is about the conversation all the patients should have with their GPs.
‘It has to be tailor made, it has to be individualised. Having a bit of a framework will help us guide the conversation more appropriately.
‘At the end of the day, we really only have a short consultation to make that decision with them. That’s why it came about.
‘The outcome is not to steer patients either way. It’s really to have an objective, scientific assessment.’
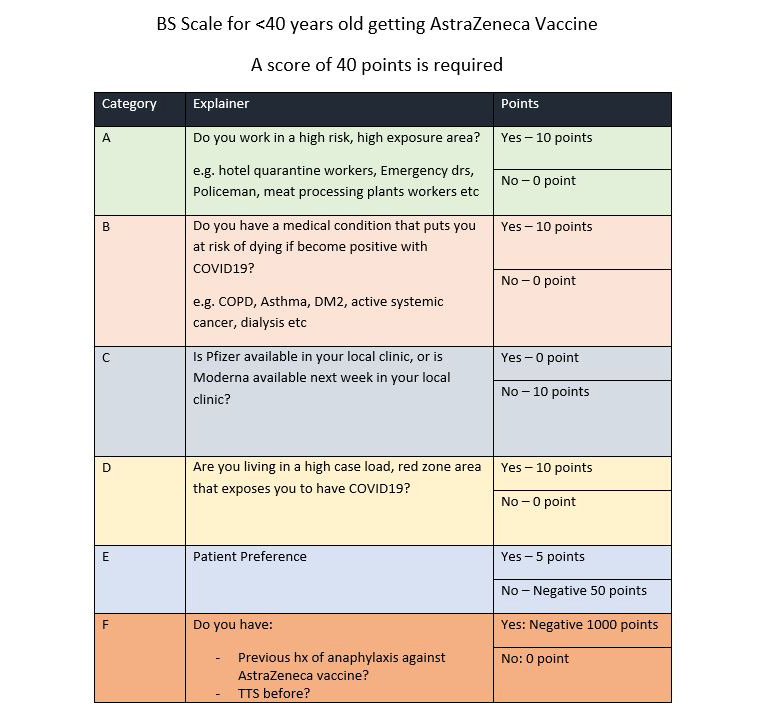
Dr Bernard Shiu’s AstraZeneca ‘matrix’ is a tool of his own creation and GPs should make their own informed decisions about COVID vaccines when discussing them with their patients.
The matrix is Dr Shiu’s creation rather than an official tool. However, for Professor Julie Leask, a social scientist at the University of Sydney whose research focuses on immunisation uptake and communication, it reflects a commendable approach to discussing the vaccine with patients.
‘This sort of thing picks up on the spirit of shared decision-making where clinicians are encouraged to talk with patients to help them understand the risks and benefits of their options, and then to work with patient to determine what is important to them about those risks and benefits,’ Professor Leask told newsGP.
Professor Leask did express some reservations about the points system used, saying some comorbidities might have a higher weighting than others.
‘[The points system] is attractive, but it’s probably enough to be talking to patients about these things and respecting the patient’s choice because there is a risk to consider,’ she said.
Assessing the matrix as ‘a really helpful set of considerations but not the full scope of them’, Professor Leask also underlined the importance of discussing the risks associated with the AstraZeneca guidance.
A paper she co-authored was this week published in the Medical Journal of Australia. It looks at approaches to communicating with patients and the wider public about COVID‐19 vaccine safety, and includes suggested strategies developed in partnership with the Collaboration on Social Science and Immunisation (COSSI) steering group.
The peer-reviewed paper concludes that communication will be a key part of the vaccine rollout.
‘Achieving high COVID‐19 vaccine coverage will be a significant challenge given Australia’s supply, access and hesitancy challenges,’ the authors write.
‘Good risk communication and support for providers and the public to make decisions about vaccination are essential as we can work towards protecting all Australians, opening our borders, and continuing to live optimally with COVID‐19.’
The paper – which was written after ATAGI updated its AstraZeneca advice for under-50s in April, but before guidance changed for under-60s in June – highlights the difficulties in messaging when official advice is altered.
‘The ATAGI recommendation on the AstraZeneca vaccine poses significant risk communication challenges for clinicians and governments,’ the authors write.
‘Even small risks associated with the AstraZeneca vaccine may be hard to tolerate in a country with limited local transmission, yet an outbreak remains almost inevitable.’
The authors recommend clinicians use risks and outcome comparisons to help patients understand the magnitude of the risks not to communicate acceptability. The paper also includes suggested prompts for when a patient is hesitant about vaccination.
Professor Leask said she will continue to push for as much clarity as possible in communicating the risks and benefits of the different vaccines.
‘That’s why we have written the MJA piece,’ she said. ‘We wanted to offer guidance to any clinician communicating with a patient about the AstraZeneca vaccine in particular.
‘The more things that can outline in really clear ways and usable ways for GPs … what the considerations are when an under-40-year-old is thinking about the AstraZeneca vaccine the better.’
Log in below to join the conversation.
AstraZeneca COVID-19 vaccines
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?