News
Guidelines questioned as research highlights COVID aerosol threat
Coughing can create 100 times more aerosol particles than oxygen therapies, increasing risk for healthcare workers who wear surgical masks.
 A study volunteer observed within the replica Perspex cone exhaling visible aerosols. (Image: Supplied)
A study volunteer observed within the replica Perspex cone exhaling visible aerosols. (Image: Supplied)
Debate around protection against aerosol particles in the transmission of COVID-19 has been reignited as Queensland faces its latest COVID outbreak, linked to two healthcare workers who contracted the virus at Princess Alexandra Hospital.
Now new research, published in Anaesthesia, has added weight to the debate and once again called into question national personal protective equipment (PPE) guidelines.
It found that respiratory activities – such as coughing and deep breathing – can create 100 times more aerosol particles than oxygen therapies, which study co-author Associate Professor Euan Tovey said could partly explain why staff on hospitals wards have around 2–3 times higher rates of infection and hospitalisation than those working in intensive care units (ICUs).
According to Associate Professor Tovey, staff in normal COVID wards are only required to use droplet protection, including a surgical mask, whereas those working in ICUs have access to more complete PPE, such as N95 or FFP3 respirator masks.
‘The coughing and laboured breathing common in patients with COVID-19 produces a lot more droplets and aerosols than is produced by patients being treated with oxygen therapies,’ he said.
‘Surgical facemasks provide inadequate protection against aerosols and staff safety can only be increased by more widespread use of specialised tight-fitting respirators [N95 or FFP3 masks] and increased indoor ventilation.’
To conduct the analysis, the researchers built a novel chamber that provides extremely clean air, in which they sat 10 healthy volunteers.
Each participant breathed into a large cone and was instructed to perform a series of respiratory activities, such as breathing, talking, shouting, coughing and exercising.
They then repeated the experiments while receiving oxygen therapies, commonly used in hospitalised patients with severe COVID-19, first through high flow nasal oxygen and then under pressure through a tight-fitting facemask.
The particles they breathed out were collected, and their number and size were measured.
What they found was that up to 100 times more aerosol particles were produced with activities such as coughing, while, contrary to guideline recommendations, aerosol particles were not found in excessive amounts during oxygen therapies, which appeared to in fact reduce aerosols.
‘As the respiratory therapies did not significantly increase aerosols, these treatments should be made widely available to patients with COVID-19 who need them,’ Associate Professor Tovey recommended.
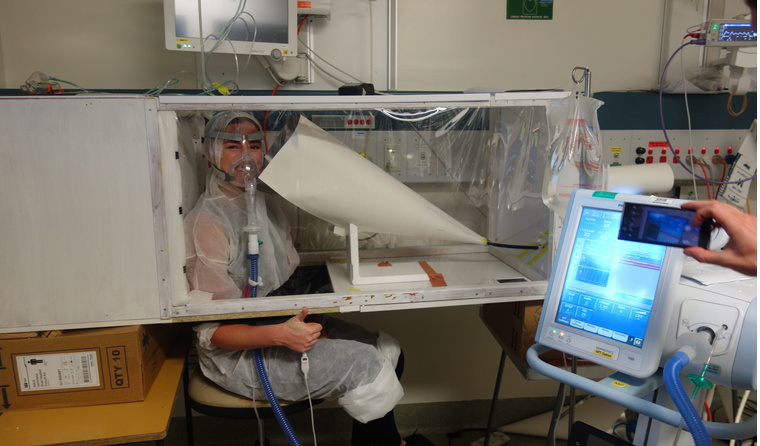
A volunteer of the study, sitting within the aerosol measuring chamber during the sampling protocol. (Image: Supplied)
As it stands, guidance on PPE from the Australian Commission on Safety and Quality in Health Care recommends those directly working with probable or confirmed cases of coronavirus only wear a surgical mask, along with disposable gloves, plastic apron/fluid-resident gown and eye protection. N95/P2 masks are only recommended for use while performing a single aerosol-generating procedure.
However, according to the study’s lead author Dr Nick Wilson from the Royal Infirmary of Edinburgh, aerosols can evade surgical masks, which are designed to protect against larger droplets, leaving healthcare workers vulnerable to smaller particles passing around the edges of the masks and being inhaled.
‘Our findings strongly support the re-evaluation of guidelines to better protect hospital staff, patients and all those on the frontline who are dealing with people who have, or are suspected of having, COVID-19,’ Professor Tim Cook, a co-author of the study from the Royal United Hospitals Bath NHS Foundation Trust, said.
Chief Medical Officer Professor Paul Kelly was asked on Wednesday during a press conference whether he thought the current guidance was sufficient in light of the Queensland outbreak.
‘I’m not sure that you’re correct in saying that … someone directly involved with the care of COVID-19 patients would be wearing only a surgical mask,’ he said.
‘But certainly, the important thing is that the appropriate PPE is being worn for those who are using it: N95 or P2 masks, that it is properly fitted. And that other protections, not just about masks, but other personal protective equipment and other procedures are followed. So that’s really important.
‘It’s really the responsibility of the healthcare facilities themselves to be following the guidance and to be protecting their staff.’
Meanwhile, Professor Guy Marks from the University of New South Wales, who also contributed to the research, said the findings have implications for the wider community.
‘The generation of both droplets and particularly aerosols by everyday breathing activities reinforces the importance of maintaining social distance,’ he said.
‘[As well as] having excellent ventilation in buildings and transport, being outside where possible and using effective masks both to protect from breathing in virus and reducing the amount of virus they spread when breathing out.’
Log in below to join the conversation.
aerosol particles airborne transmission coronavirus COVID-19 PPE