News
Hidden impact of bleeding disorders
This week is Bleeding Disorder Awareness Week. Haemophilia Foundation Australia is raising awareness about the inherited condition and its impact on the sufferers and their families.
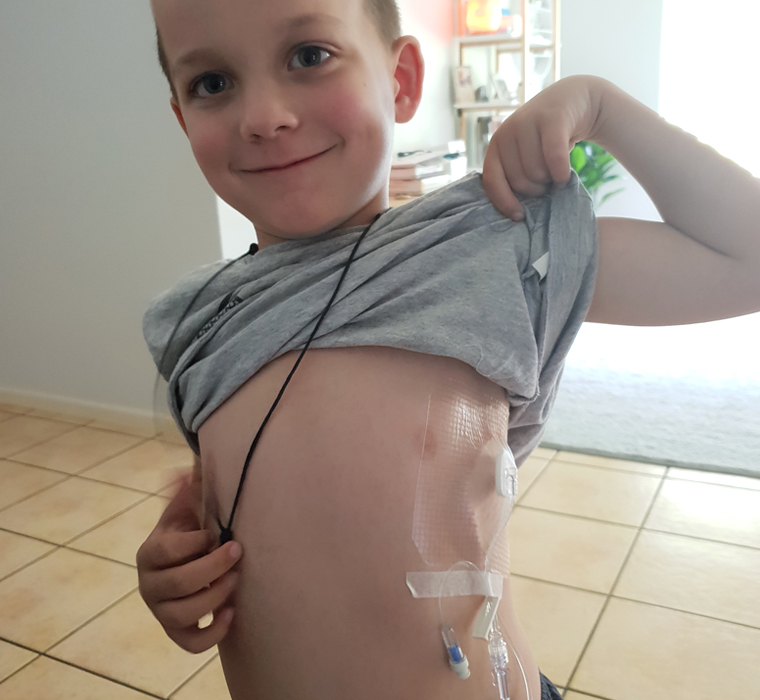 Mason was diagnosed with a severe form of haemophilia when he was three months old.
Mason was diagnosed with a severe form of haemophilia when he was three months old.
Mason was just three-months old when his mother, Jacqui Bradshaw, noticed something wrong with his left leg.
The GP suspected a fracture and put the baby in a half plaster cast.
But when Mason seemed to get worse, Jacqui was sent off to the children’s hospital where things got really bad.
‘… The first thing that the [emergency doctor] did was strip Mason and check the rest of his body,’ Ms Bradshaw told newsGP.
‘He had a little yellow bruise on his rib. I was a first-time mum and I thought, “maybe he’s rolled over on a toy … and it’s caused a bruise.” I didn’t realise babies didn’t normally bruise and that was abnormal.’
The ED doctor diagnosed Mason with a spiral fracture and told Jacqui she would be investigated for child abuse.
‘She said to me, “any child under the age of two-years-old that comes in with a broken bone automatically gets red-flagged by child protection, and you are not able to leave the hospital until Mason has a full leg plaster on”,’ Ms Bradshaw said.
‘[She said], “You will be escorted down to child protection for a formal interview”.
‘It was terrifying.’
Ms Bradshaw finally left seven hours later, but was asked to come back for more tests when Mason was diagnosed with a bleed into the back of his knee muscles due to a severe form of haemophilia.

L to R: Mason, Todd, Jacqui and Beau. Jacqui Bradshaw is studying nursing to be able to better help other children with a bleeding disorder.
Director of the Haemophilia Treatment Centre at The Alfred Hospital, Melbourne, Associate Professor Huyen Tran told newsGP that haemophilia is a hereditary bleeding disorder.
‘[There are] two typical forms, known as Haemophilia A and Haemophilia B,’ Associate Professor Tran said.
‘Both of these conditions are X-linked, so predominately, with some rare exceptions, it’s really a boy’s disease. Men manifest with bleeding symptoms.’
Associate Professor Tran said haemophilia is still quite rare, with the worldwide prevalence of Haemophilia A being about one in 10,000, while Haemophilia B is a lot less common, with about one in 30,000 affected.
‘The standard of care for haemophilia today has been Factor 8 or Factor 9 treatment (both amplify the clotting system to varying degrees) … for which the patients have to inject it into their veins,’ Associate Professor Tran said.
‘In most severe forms of both haemophilia, these patients would be taught how to self-administer these factors concentrated … three times a week.
‘So if you give it yourself three times a week in a lifetime, you’d be giving yourself a needle over 12,000 times.’
But Associate Professor Tran said there are many novel treatments being discovered for patients suffering from the disorder.
‘The initial new therapy is … extended half-life or EHL, it just means we lengthen the half-life of these products, which means the patient can reduce the number of times they need to administer each week,’ he said.
‘Beyond that we have got a drug called Emicizumab, it is an anti-body that mimics the function of Factor 8. This drug can be given weekly or once fortnightly.’
Associate Professor Tran said gene therapy was also on the horizon which treats the patient with a viral vector that contains a code telling the liver to make the missing Factor 8 or Factor 9.
‘The crux of the problem of haemophilia … is that you bleed and you bleed into joints and muscles,’ he said.
‘So if you get haemophilic arthropathy then you are going to have a very poor quality of life.’
Haemophilia Foundation Australia Executive Director Sharon Caris said haemophilia is an invisible disorder with most people not realising the impact on the sufferers, including the fear of a spontaneous bleed.
‘One terrific thing these days is that people can be treated and bleeds can be stopped, but … it is a hidden impact in lots of ways,’ Ms Caris told newsGP.
‘People see young kids and young adults looking in fairly good shape, but in fact they might have joint disease and are certainly at risk of joint damage and muscles if there bleeds aren’t under control, so it develops into arthritis.’
Ms Bradshaw said she has started studying nursing so she can help her son and others like him.
‘The whole diagnosis has changed our family. Although, it is hard and difficult, especially for Mason to go through the things that he goes through, but it has definitely made me, as a mum … I feel stronger, I feel more in control, I feel I can walk in into any hospital setting and advocate for my child,’ she said.
‘Oncology and haematology nurses are inspirational people … the way they handle their job and the way they care for children.
‘I could offer a different level of care being a nurse and a mum of a child who has a chronic illness.’
Bleeding Disorder Awareness Week runs from October 7–13. Visit Haemophilia Foundation Australia for more information and support.
Bleeding Disorder Awareness Week bleeding disorders Haemophilia Haemophilia Foundation Australia
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?