Feature
How close is Australia to becoming the first country to end HIV transmission?
New prevention drugs, better testing and antiretroviral therapy have put us within reach of ending transmission of HIV in Australia. But challenges remain.
 Increased testing has been a factor on helping to bring the elimination of HIV transmission in Australia within reach.
Increased testing has been a factor on helping to bring the elimination of HIV transmission in Australia within reach.
There is no magic cure for HIV. Yet ending transmission of the virus in Australia is now entirely possible.
How can this be?
In 2014, the Federal Government set a target of virtually eliminating new HIV cases by 2020. It was an ambitious target to be sure, as only two years earlier new HIV infection rates had hit their highest rate in 20 years.
Yet that target is becoming within reach, courtesy of a number of factors, including this year’s listing of the breakthrough preventive drug treatment PReP on the Pharmaceutical Benefits Scheme (PBS), increased testing, effective antiretroviral drugs, and safe-sex messaging.
Australia’s three most populous states have all publicised recent rapid drops in HIV transmission.
Rates of new infection are down 22% from last year in Victoria, with 130 new cases of HIV in the year to date, compared to 167 for the same period last year. New South Wales had a 27% drop in the April–June quarter compared to the same period in 2017, and Queensland recently announced it would no longer list AIDS as a notifiable health condition after new cases of AIDS fell to just 12 across the state in 2017.
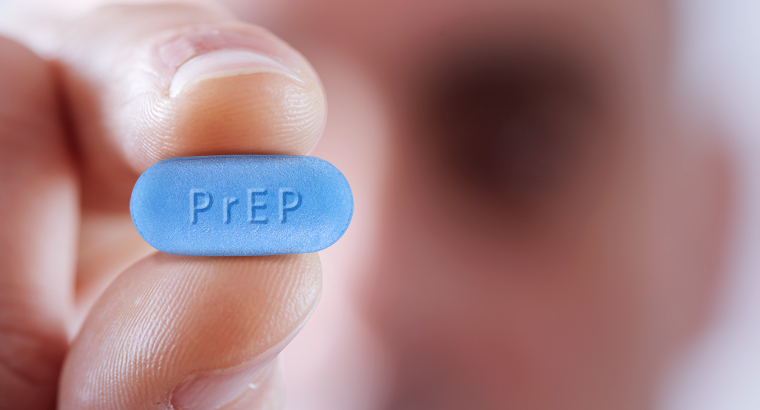 Prevention treatment PReP (pre-exposure prophylaxis) being listed on the PBS has been cited as a major factor in the continuing decrease in Australia’s rates of HIV transmission.
Prevention treatment PReP (pre-exposure prophylaxis) being listed on the PBS has been cited as a major factor in the continuing decrease in Australia’s rates of HIV transmission.
Darryl O’Donnell, Australian Federation of AIDS Organisations (AFAO) Chief Executive, told newsGP that while the nation is making serious inroads against HIV transmission, it is still falling short of the 2020 goal.
‘The next tranche of national surveillance data is likely to show a serious decline in the transmission rate,’ he said. ‘PrEP is a key factor in this progress. It’s something that gay men in particular are embracing and have called for over a long period.
‘However, it’s important to note that testing among gay and bisexual men is also at an all-time high. Community knowledge of the importance of treatment and the fact it makes HIV non-transmissible is also critical.
‘Virtually eliminating HIV transmission by 2020 is very ambitious and it’s unlikely it can be achieved in so short a time. Achieving it will require significant reinvestment in education programs, the skills of the HIV workforce, nationally consistent policy and sophisticated use of big data.
‘We also need to take stock of very concerning increases in the rate of HIV among Aboriginal and Torres Strait Islander people – now double the rate of non-Indigenous Australians.’
There are rising concerns regarding these increasing rates of HIV in Aboriginal and Torres Strait Islander communities, with a 33% surge from 4.8 per 100,000 people in 2012 to 6.4 per 100,000 in 2016.
‘We have had the tools to prevent, diagnose and treat HIV for some time. However, medicine is only as powerful as the political and financial commitment to ensure it reaches those in need,’ Mr O’Donnell said.
Around 25,000 people currently live with HIV in Australia. Most are on antiretroviral therapy, which can slash the viral load to undetectable levels.
An influential 2017 Australian study by the Kirby Institute found that HIV-positive men who have sex with men who were on antiretroviral therapy and had an undetectable load do not transmit the virus to their partners. The study followed a larger 2016 European PARTNER study that had very similar results.
Sexual health GP Dr George Forgan-Smith told newsGP that Australia is heading in the right direction, with PReP crucial to the elimination effort.
‘We’ve seen a clearly demonstrated drop in transmissions, and PReP has been the vital key,’ he said.
‘The other crucial thing is that we now know undetectable equals untransmittable.
‘We clearly know that people living with HIV and on successful treatment with an undetectable viral load are absolutely unable to transmit to partners. That means women with HIV [and an undetectable viral load] can have babies with no worries of transmitting it.’
Dr Forgan-Smith said a focus on making sure PReP is as widely available as possible is required to eliminate HIV transmission entirely.
‘For Indigenous people, transgender people, those who aren’t able to afford PReP – we have to work harder to make sure it’s available to all people at risk, not just gay white men,’ he said.
‘We need to address the huge disparity in HIV testing and treatment [across the country]. We can’t have a cure without addressing the 10% left behind.’
HIV HIV prevention PReP sexually transmissible infection
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?