Feature
How one US doctor made a change to help tackle America’s opioid crisis
When this emergency doctor was unable to help a patient experiencing addiction, he looked deeper.
 US emergency physician Dr Alister Martin described GPs as ‘critical’ to addressing Australia’s growing opioid problem.
US emergency physician Dr Alister Martin described GPs as ‘critical’ to addressing Australia’s growing opioid problem.
Dr Alister Martin had been a doctor for all of a week when it happened.
It was a Friday night and the emergency department (ED) at Massachusetts General Hospital was busy.
A woman in her 30s came in at around 2.00 am. She told Dr Martin she’d been sent home with oxycodone after a bad ankle fracture six weeks previously.
She soon found she could not feel normal without her medication. And so it began.
The patient found a leftover stash in the bathroom cupboard. She then asked friends and family. When she ran out of options, she found her first drug dealer and plunged straight into a full-blown dependency.
After that six-week dive into opioid addiction, she had come back to herself. She told Dr Martin that she had called her dealer and said she wanted out, that he should erase her number, that she needed to look after her two kids better. An hour later, there was a knock at the door. Her dealer had brought her 15 pills for free to ‘help her recover’ – after all, she had been such a good customer. Her husband, appalled, sent him away.
‘That’s when she realised she had a problem and that she could not do it alone,’ Dr Martin told newsGP.
‘So she came to me at 2.00 am on a Friday and I heard her story and I said, “Of course we can absolutely help you get your life back on track. We’ll admit you and get you treated”.’
But when Dr Martin talked to the senior consultant, the response he got was simple: It’s not what we do here. She has to be discharged, and she has to find help elsewhere. We can’t solve every problem here.
Here, of course, was the largest hospital in the state, and the teaching hospital for Harvard Medical School. And Massachusetts was the number one US state for emergency department visits for patients with an opioid dependency.
Dr Martin knew, however, that there was nowhere else for her to go.
The US was in the grip of a well-documented opioid addiction crisis, with more than two million people dependent on strong prescription opioids such as OxyContin. More than 130 people were dying each day from overdose. Waiting lists at treatment centres were out of control. And America has a growing shortage of primary care physicians, with a predicted shortfall of up to 49,300 doctors by 2030.
So Dr Martin took a closer look at the problem.
Get Waivered
After medical school, Dr Martin spent two years getting his Master’s degree in behavioural economics. That lens gave him the idea to look closely at the issue.
Given opioid-substitution therapy had long been well established, why weren’t more hospital doctors getting involved in the opioid public health crisis? Why were only one in 10 Americans with an opioid dependency able to access treatment?
Dr Martin found the problem in EDs could be boiled down to three behavioural reasons: hassle bias, a lack of social norms, and salience.
Emergency physicians could be involved in treating opioid dependence by prescribing buprenorphine, a key pharmacotherapy treatment. But becoming a prescriber required them to apply for a waiver from the Drug Enforcement Administration, which included completion of an eight-hour course. It was a bureaucratic hurdle. A hassle.
‘If there are extra steps that have to be done, that makes it less likely someone is going to complete an action, even if they have the motivation to do it,’ Dr Martin said.
Secondly, there were no social norms around treating opioid dependency. Doctors didn’t have a sense that this was something they should be doing.
And, thirdly was salience.
‘It’s basically the idea that attention-grabbing behaviours make us more likely to do that action,’ Dr Martin said.
So Dr Martin devised the Get Waivered campaign in an attempt to alter the ‘we-don’t-treat-addiction’ status quo.
Launched in December 2017, the campaign worked remarkably quickly, with 95% of all emergency physicians in Dr Martin’s hospital getting their waiver and thus gaining the right to prescribe pharmacotherapy. By contrast, only 1% of emergency physicians have a waiver across the entire US.
‘In the emergency department, you don’t get to see your successes. You don’t get to see the people you took care of who are now 10 years into recovery because they have no reason to come back,’ Dr Martin, who is now Chief Resident at the Harvard Affiliated Emergency Medicine Residency, said.
‘So emergency doctors develop this unfortunate worldview – because they see people who have relapsed or overdosed – that these patients don’t get better.’
Better still, Massachusetts passed a state law in July last year that requires all hospitals to be able to treat opioid addiction in EDs. The far-larger state of Texas is now looking at a similar approach.
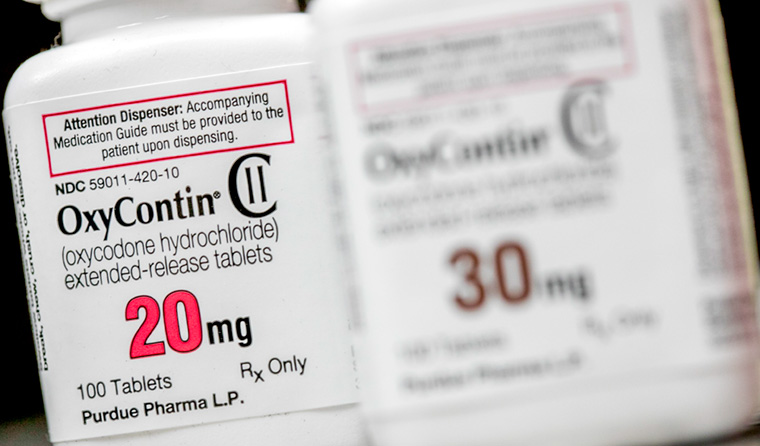
More than two million people in the US are dependent on strong prescription opioids such as OxyContin. (Image: Kris Tripplaar)
A dangerous path
Dr Martin was recently in Sydney for the SMACC (‘Social Media and Critical Care) conference.
He warned that Australia – where deaths from opioid misuse have nearly doubled in 10 years – could be going down America’s route.
‘What we saw in the US was this slow upward trend that became a rapid increase in lives lost. And one thing that changed was when access to opioid prescriptions was limited,’ he said.
‘As the number of pills floating around decreased, people switched to heroin, which comes with a huge risk of overdose. And now we have fentanyl, which is multiple times stronger than heroin.
‘I see patients in the ER who say, “I don’t want to do this anymore. I don’t know what I’m using and it’s basically a life-or-death role of the dice. If it’s heroin, I’ll probably be okay. But if it’s fentanyl, I won’t make it another night”.
‘Patients are actually afraid. They’re coming in saying they don’t know where else to go and that they need help.’
Dr Martin said that part of the challenge was overcoming doctors’ resistance.
‘Doctors had to learn that they do have the capacity to treat this, and that patients get better in ways we don’t see in other diseases,’ he said.
‘If you give a statin to reduce cholesterol, the patient might get a little more life. But with this disease, you get decades. You change the course of someone’s life – and of future generations in that family.’
Dr Martin recently had a win. One of his regular patients was a lawyer in her 30s who had struggled with oxycodone dependence for years, but could not shake it. One day she came in, saying she’d been nauseous, fatigued and out of it in the preceding weeks. It turned out these symptoms were evidence of pregnancy.
She told Dr Martin that now she simply had to change.
‘She said, “I know I have no choice – for the future of my kid, I have to do this”,’ Dr Martin said.
His colleague got her started on buprenorphine.
Three months later, Dr Martin checked the patient’s medical records from the hospital’s in-house Bridge Clinic, staffed by primary care physicians. His patient was recovering well, and her pregnancy progressing.
‘It wasn’t until I told my colleague that he found out the outcome. And the look I got from him – it was like that’s what we all get into medicine for, that look of I was able to make a difference.’
Dr Martin said family physicians – the US equivalent of GPs – are vital partners in the fight against dependency.
‘We have a saying in the ER, “We’re only as effective as our outpatient follow-up options”. We can’t be effective in treating this disease if it’s only ER doctors doing this,’ he said.
‘Now, patients get a three-day go-pack of buprenorphine when they leave. But what happens on day three? Someone has to be there on the other side to catch them.
‘So it’s critical that family physicians – who know the patients well – are partners and take on the work afterwards. It’s so critical.’
dependency opioids pharmacotherapy
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?