News
‘It’s mis-sold as an insurance policy’: Fertility expert on egg freezing
Dr Raelia Lew explores what GPs need to know about elective egg freezing.
 Fertility expert Dr Raelia Lew is keen to dispel the myth that egg freezing is a guarantee of future pregnancy. (Image: Melbourne IVF)
Fertility expert Dr Raelia Lew is keen to dispel the myth that egg freezing is a guarantee of future pregnancy. (Image: Melbourne IVF)
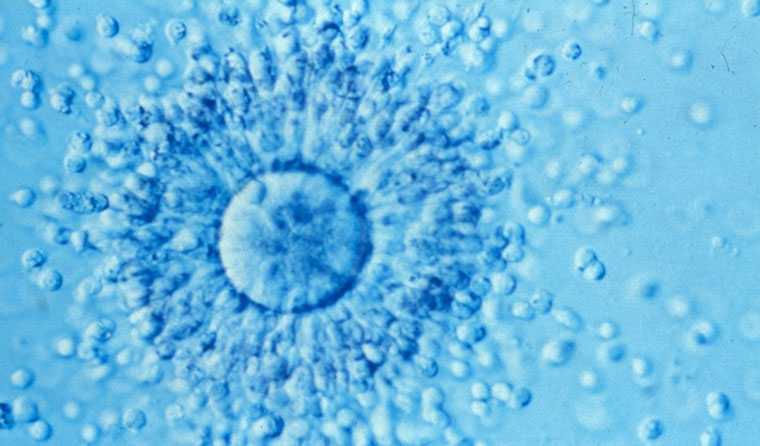
Egg freezing – oocyte vitrification – is the process of storing a woman’s unfertilised eggs in order to allow her to try to conceive at a later date.
It has been considered a non-experimental therapy in Australia since 2012, and fertility expert Dr Raelia Lew from Melbourne IVF has been performing the procedure since 2014.
While stories are filtering more and more into mainstream media, Dr Lew said she is concerned about some of the myths that are circulating about the process.
For example, patients often come to Dr Lew assuming that having their eggs frozen means they can go on and have a baby whenever they choose.
‘I think it’s mis-sold as an insurance policy,’ she told newsGP.
‘Egg freezing is not a guarantee of future pregnancy.’
Instead, according to Dr Lew, the process simply allows a woman to create a finite resource of her own oocytes at her current age. And a woman’s age is a key factor in affecting her chances of becoming pregnant.
According to Dr Lew, there has been a significant media focus on the age of 35 being a magical fertility number, with women being told their fertility declines after that age.
Consequently, many women choose to look into fertility options around this time.
Instead of waiting until a woman is 35 before referring her to a fertility expert, Dr Lew believes it is best to start the process around the age of 30.
‘In terms of egg freezing, clinically, what goes in really dictates what comes out,’ she said.
‘So women who put a high number of healthy younger eggs into the freezer will have a better prognosis long-term for utilising those eggs to have a baby.’
Dr Lew explained that a female foetus makes her own lifetime supply of oocytes at around 6–12 weeks’ gestation.
‘Those cells have to last the distance and they’ve got a limited metabolic potential, so there comes an age when they reach their shelf life, and that happens differentially,’ she said.
‘By the time we’re 35, at least 50% of our eggs will generate aneuploidy embryos.
‘It’s more and more the exceptional, rather than the average, egg that can make a baby [at that age and older].’

Dr Lew believes it is important to explore a ‘patient’s goals and to discuss other options’ before referring them to a fertility expert.
Before referring a patient to a fertility expert, Dr Lew said it is also important for GPs to discuss a patient’s long-term fertility plans.
‘What I really do is discuss with the patient is all of their treatment options for family planning, because we’ve got to establish what their goals are,’ she said.
For instance, Dr Lew has found it common for a patient to present for egg freezing because she does not currently have a partner, but is hoping to become a mother soon.
‘I think it’s really important for GPs to understand that when you send a patient to a fertility expert to discuss egg freezing, what is considered the best practice is to really explore that patient’s goals and to discuss other options,’ she said.
‘Because I do have a certain proportion of the cohort of women who come to talk about egg freezing who ultimately decide to have a baby with a sperm donor and become a single mum.’
Such discussions are important to not only ascertain a woman’s fertility plans, but to also help her avoid a costly, potentially unnecessary procedure.
Elective egg freezing is expensive in that it attracts no Medicare rebate, so women who choose to undergo the procedure will be out-of-pocket around $7000, according to Dr Lew. Of that, $1500–2000 goes towards the cost of hormonal medicines, which are not listed on the Pharmaceutical Benefits Scheme (PBS).
Patients with medical indications, such as cancer patients about to embark on chemotherapy, can attract Medicare eligibility for oocyte preservation.
In terms of the actual process of freezing, a woman self-injects hormones for approximately two weeks before egg retrieval to stimulate oocyte maturation. Most women produce around 10 eggs in an average month, and it may take 2–3 cycles to produce enough eggs for storage.
Retrieval is then performed under anaesthetic as a day procedure, and takes around 20–30 minutes.
Dr Lew aims to freeze around 20–30 eggs. Eggs are frozen at around – 1700C, and thawed if a woman presents wanting to use them for fertilisation.
The upper age limit at which Dr Lew will thaw a woman’s eggs for IVF is 51 years.
Because the procedure is relatively new, Dr Lew said it is not possible to give exact figures regarding how many women who have undergone egg freezing have then gone on to use those eggs to produce a successful pregnancy. There is a 6–12% chance of live birth per oocyte vitrified.
Those statistics may seem bleak, but the numbers are not as daunting on closer inspection.
‘It’s important to know that, when it comes to vitrified eggs, if they survive the thaw they act like fresh eggs, so statistically we see very similar fertilisation rates to fresh eggs,’ Dr Lew said.
The difficulty is that some eggs will be lost in the thawing process.
‘We see similar embryogenesis rates but, overall, we get fewer blastocysts because we have fewer eggs to play with,’ Dr Lew explained.
In Dr Lew’s experience, a minority of the patients who have elected to have their eggs frozen have returned to attempt fertilisation.
‘Less than 12% have come back to use them,’ she said.
Of those who have returned, however, Dr Lew has ‘lost count’ of how many successful pregnancies have resulted, adding that this year alone, she has had five women become pregnant from their own frozen eggs.
egg freezing fertility pregnancy
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?