News
Less than 10% of under-fives vaccinated against flu
As influenza cases rise sharply, a poll conducted by the Royal Children’s Hospital in Melbourne suggests many parents are unaware of the risks.
 Only 151,189 children aged 0–5 have had influenza vaccinations recorded on the Australian Immunisation Register in 2022.
Only 151,189 children aged 0–5 have had influenza vaccinations recorded on the Australian Immunisation Register in 2022.
One in two children may not get vaccinated against flu this season, in part due to parents’ misconceptions about the vaccine, a new poll suggests.
According to a survey of 2002 parents by the Royal Children’s Hospital (RCH), the results of which were published on Wednesday (25 May), more than a third said they were unaware of how severe influenza could be among children.
Parent responses to the survey also suggested only around half of Australian children would be vaccinated against flu this winter.
Their responses indicate the highest uptake is likely among children under the age of five, who are also covered by free vaccinations under the National Immunisation Program.
However, Australian Immunisation Register (AIR) data suggests fewer than 10% of children in this cohort have been vaccinated so far in 2022.
Up to 22 May, only 151,189 children aged 0–5 have had their vaccinations recorded on the register, which equates to 9.7% of 0–4-year-olds when compared to Australian Bureau of Statistics population data from 2020.
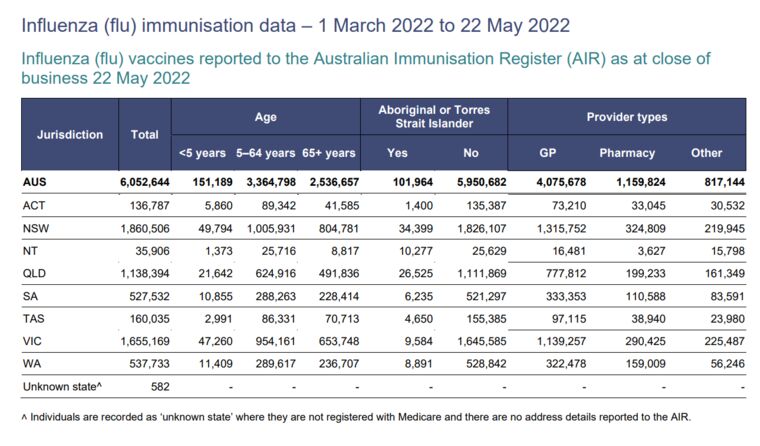 Australian Immunisation Register data on influenza vaccinations. (Source: Department of Health)
Australian Immunisation Register data on influenza vaccinations. (Source: Department of Health)
The research also suggests that cost could be a barrier to vaccination for more than a quarter of parents, with 27% citing that as a factor.
The survey results were released at the same time as states and territories across the country are reporting a sharp spike in influenza case numbers, with hospitalisations also on the rise as the disease embeds itself in the community after a prolonged absence due to COVID-19.
For Dr Anthea Rhodes, a paediatrician and Director of the RCH National Child Health Poll, the spread of infections underlines the urgency for families to come forward for vaccination.
‘[According to the poll] a third of parents are experiencing some vaccine fatigue,’ Dr Rhodes told newsGP.
‘They feel like their children have had too many vaccines already and that is contributing to their reluctance to go ahead and vaccinate against flu.
‘That’s understandable for parents, we’ve certainly asked a lot of our community and each other to stay safe from COVID.
‘But we really don’t want to see parents now skipping the flu vaccine and landing in a situation where their child becomes seriously unwell from something that may have been preventable.’
Dr Rhodes said the survey results suggest that general practices could also play a further educational role in vaccine uptake.
More than half of those questioned were unaware of an assessment by the Australian Technical Advisory Group on Immunisation (ATAGI) that it is safe for flu vaccines and COVID-19 vaccines to be administered at the same time.
‘GPs are really critical as a way to deliver flu vaccines to kids,’ Dr Rhodes said.
‘That contact with families can provide that reminder, education and information to let families know that flu is here, and that it is important for children to have a flu vaccine.’
Flu back ‘with a bang’
Professor Ian Barr, Deputy Director of the World Health Organization Collaborating Centre for Reference and Research on Influenza at the Doherty Institute, said the timing of the surge contrasts to pre-pandemic patterns.
‘It is definitely earlier, [although] we did see an early season back in 2019, which everybody’s forgotten about by now,’ he told newsGP.
‘It’s come early, and it’s come with a bang. Normally, we wouldn’t see this level of activity until probably June or July.’
Another distinctive aspect of the season so far is the widespread presence of two different strains of influenza A, which indicates a significant likely impact on both children and adults.
‘[The] two different types of influenza A circulating ensures that all age groups will be affected,’ Professor Barr said.
‘That’s something a little unusual. Often, we see one virus predominate over the other but now we’ve got both co-circulating at reasonable levels.
‘The children will be more affected by the H1 pandemic strain, and the H3 affects all age groups.’
Professor Barr reiterated the urgency of vaccination, highlighting what he called a ‘pretty pathetic’ level of coverage so far.
According to the AIR, 42% of flu vaccinations administered since March have been among over 65s (2,536,657), while only 2% have been given to children younger than five.
GPs have been responsible for more than two thirds of the 6.05 million influenza vaccinations administered so far in 2022.
Professor Barr said he encourages general practices to consider taking swabs and sending them in for testing if they are unsure whether a patient has COVID-19 or influenza.
He also believes it is likely to be a severe flu season.
‘It clearly is starting to bite in terms of hospitalisations,’ Professor Barr said.
‘That’s not unexpected with more cases, we have a proportion of them that will end up in hospital, ICU – and a small proportion will die.
‘All are characteristics of a significant season.’
Vaccine access
In response to the rising case numbers, and a sharp spike in hospitalisations, Queensland Health has expanded cost-free access to the community as a whole this week.
NSW Health is reportedly ready to make a similar move from next week, while Victorian Premier Daniel Andrews has also said his government is considering the option.
After urgent talks with Queensland Health, the college has now received confirmation that GPs will be reimbursed $21.95 per dose for private flu vaccines until 30 June.
Dr Michael Tam, a Sydney GP and member of the RACGP Expert Committee – Quality Care (REC–QC), believes the decision to make the vaccination free to a wider population should have been taken earlier.
‘The challenge is that some of the decision-making about that seems to have been fairly reactive,’ he told newsGP.
‘These are logistics and practical things that really need to be planned.’
Dr Tam is also expecting the already rising level of influenza-like-illness presentations to further increase.
‘When flu season first hits … most of the time you don’t see too many people with influenza-like illness,’ he said.
‘Then all of a sudden there are tonnes of people. I think we’re going to start [seeing] that quite soon.’
Dr Tam also warns that the ongoing pandemic is complicating care.
‘The dimension of COVID has, I think, made it more difficult for general practices to support people presenting with acute respiratory symptoms,’ he said.
‘There [are] costs involved with the PPE and even just the availability of the PPE.
‘The GP respiratory clinics are doing a good job, but their capacity can be fairly easily saturated, especially if in their locality not only are people getting COVID, but suddenly a lot of people are also getting influenza-like illness at the same time.
‘It’s going to be challenging.’
The RACGP has promotional material, including posters, for GPs to let patients know they are providing the flu vaccine, available on the RACGP website.
ATAGI advice on the administration of flu vaccines is available on the Department of Health website.
Log in below to join the conversation.
children COVID-19 influenza vaccination
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?