Column
Managing hyperkalemia with dietary changes
GPs and dietitians can work together to better manage hyperkalemia in general practice.
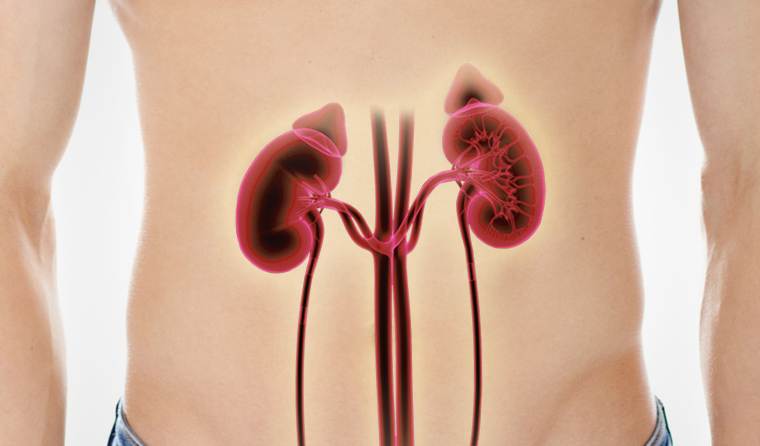 Given close to 1.7 million Australian adults live with chronic kidney disease, GPs are likely to see patients with hyperkalemia.
Given close to 1.7 million Australian adults live with chronic kidney disease, GPs are likely to see patients with hyperkalemia.
Chronic kidney disease (CKD) is common in Australia. Approximately one in 10 adults (close to 1.7 million people) live with the condition,1 and one in three is at risk of developing CKD.2 Excretion of potassium is a key function of the kidney; when a person’s kidney function declines, it is likely their GP will observe persistent high serum potassium readings (hyperkalemia).
What dietary advice is needed for hyperkalemia? Can it be prevented?
Risk factors
The stage of CKD is important in the likelihood of hyperkalemia. When CKD progresses, the kidneys’ ability to excrete potassium declines and hyperkalemia usually starts at around CKD stage 3b (<44 ml/min).
Once the kidney function has reduced to around stage 3b, there are four main reasons hyperkalemia could develop:
- Medications – several medications increase the risk of hyperkalemia, including angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers (ARBs), and aldactone (a potassium-sparing diuretic). A reversible reduction in glomerular filtration rate occurs when ACEs or ARBs have been initiated, and a rise in serum potassium of 0.5 mmol/L is expected. There is a general consensus within the nephrology community that hyperkalemia will occur in the first six weeks after commencement of an ACE or ARB, and that ACEs and ARBs should be continued with appropriate monitoring.3
- Untreated metabolic acidosis – to compensate for the build-up of excessive amounts of metabolic acids, the cells will take up some of the hydrogen ions. This exchange results in a release of some of the potassium from within the cells, leading to an increase in blood levels of potassium.
- Constipation – this results in potassium reabsorption from the stool and increases the risk of hyperkalemia, especially if treated with aperients such as Nulax or liberal use of dried fruit.
- Excessive dietary potassium intake – this can lead to hyperkalemia for patients with impaired renal function.
Dietary modification
Evidence indicates that a low-potassium diet should be initiated when serum potassium is persistently >6 mmol/L4 or there are additional risk factors, such as CKD at stage 3b or lower in conjunction with an ACE inhibitor or ARB.
3
Low-potassium dietary modifications are based on a person’s body weight (usually 1 mmol/kg). People of a low body weight require a tighter restriction than larger, more muscular individuals.
It is virtually impossible (and unhealthy) to have a potassium-free diet. High levels of potassium are found in a wide range of staple foods and inappropriate restriction results in reduced dietary variety and constipation. Additionally, it is not compulsory for Australian food manufacturers to declare the potassium content of their products.
Some staples high in potassium include:
- fruit – bananas, apricots, mangoes, grapes (in large quantities), kiwifruit, dried fruit, all fruit juices
- vegetables – potato, sweet potato, pumpkin, tomato, avocado, cauliflower
- breads and cereals – bran-based cereals, breads with bran or large amounts of wholegrains
- dairy products – milk, yoghurt, custard, ice cream
- protein sources – nuts, large serves of meat, chicken and fish.
There are also several hidden sources, including salt substitutes and strong coffee.
Dietary management
All patients with CKD should be referred to an
accredited practising dietitian (APD) to learn about restrictions to dietary potassium, as well as additional dietary modifications to help manage other symptoms of CKD and prevent its progression.
Practical suggestions to help manage hyperkalemia in the short term:
- Limit fruit intake to two serves per day, choosing low-potassium options such as apples, strawberries, mandarins, passionfruit, pear or a small slice of watermelon.
- Limit fruit juice to no more than 150 ml per day.
- Drain liquid from tinned fruit (and do not drink the juice).
- Reduce the serving size of starchy vegetables such as potato, sweet potato or pumpkin to half a cup each day (augment meals with low-potassium choices such as pasta, white bread, rice, carrots, beans, corn, asparagus, zucchini).
- Peel and boil vegetables to leach some of their potassium (the water will be high in potassium and should not be consumed; similarly, vegetable soups are high in potassium and should be avoided).
- Avoid large serves of tomato products (eg paste, puree, soup, etc).
- Avoid cereals high in bran.
- Do not use salt substitutes.
- Avoid items such as liquorice, chocolate, potato chips and strong coffee.
- Limit dairy products to 200 g of yoghurt or 300 ml of milk per day (but not both).
chronic-kidney-disease hyperkalemia
newsGP weekly poll
As a GP, would you benefit from further education about identifying and supporting patients impacted by intimate partner violence?