Opinion
Medicinal cannabis: A GP examines the evidence
GP and integrative medicine practitioner Dr Vicki Kotsirilos writes for newsGP about existing evidence for the provision and use of medicinal cannabis.
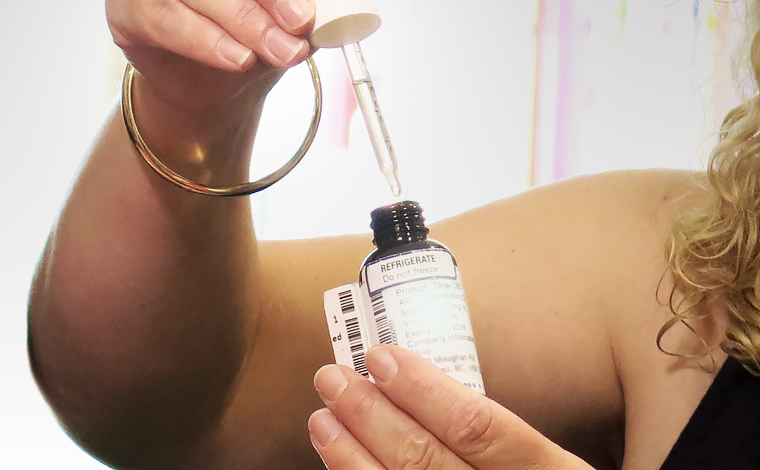 Medicinal cannabis products are oil-based or liquid-based cannabis or cannabinoid extracts that are more slowly absorbed with oral administration. (Image: AAP/Alex Murray)
Medicinal cannabis products are oil-based or liquid-based cannabis or cannabinoid extracts that are more slowly absorbed with oral administration. (Image: AAP/Alex Murray)
Due to strong demand and lobbying from patient advocacy groups, Australia’s federal and state governments improved lawful accessibility of medicinal cannabis in 2016. This has put increasing demands on many Australian GPs to prescribe medicinal cannabis products for their patients.
The Therapeutic Goods Administration (TGA) defines medicinal cannabis products as ‘a range of cannabis preparations intended for therapeutic use, including pharmaceutical cannabis preparations, such as oils, tinctures and other extracts’.
These products should not be confused with marijuana smoking for recreational use (an important social issue of its own), usually heated and inhaled with tobacco. This is a harmful process that causes serious health problems, such as respiratory disease, addiction, depression, anxiety and psychotic episodes, the latter mainly seen in young people with frequent use. The smoking of any substance is likely to have an adverse effect on health and cause respiratory diseases.
Medicinal cannabis products are cannabis or cannabinoid extracts in very small doses. They are oil-based or liquid-based and are more slowly absorbed with oral administration. Other methods of administration include transdermal, oro-mucosal spray and vaporising. They are usually not heated, (apart from vaporising methods with lower temperature heats), usually swallowed, absorbed sublingually or applied transdermally. They do not share the same risks as the recreational variety and are only recommended in unwell patients for therapeutic purposes.
Medicinal cannabis products are emerging around the world as important agents for relieving distressing symptoms in people with certain conditions, especially if conventional medicines have not been effective.
The cannabis plant consists of a number of active constituents, including terpenes and many cannabinoids. The delta-9 tetrahydrocannabinol (THC), cannabidiol (CBD) and cannabinol (CBN) are the most well known and active components and their ratios determine choice of product for treatment of disease.
Medicinal cannabis products in Australia are now accessible only to appropriate patients for certain medical conditions. Anecdotal evidence suggests overseas medical doctors and Australian GPs are finding them of value, particularly for patients who have suffered side-effects and are not finding symptomatic relief with their usual medications and treatments.
The majority of patients seeking medicinal cannabis products are those with chronic severe pain, and those who are experiencing terminal illnesses (such as cancer) and intractable conditions (such as spasticity associated with multiple sclerosis and severe uncontrolled epilepsy).
In Australia, Nabiximols (Sativex oromucosal spray), an extract of cannabis, is available on the Australian Register of Therapeutic Goods (ARTG) on authority by specialists for its clinical benefits of muscle relaxation for spasticity associated with multiple sclerosis, if intolerant or not responding to anti-spasmodic medication.
International scientific research suggests there may be clinical benefits to support the use of medicinal cannabis products for certain medical conditions. There is no evidence it is more harmful or riskier than opiates, which are widely prescribed by GPs and may actually help reduce mortality from opioid overdose.
Due to heterogeneity of medicinal cannabis products (the mixture of cannabinoids can change from crop to crop), dosages being tested in studies and research methods varying between studies, it is still not clear what products, strains, types, dosages and strengths of these products are particularly useful for which conditions. This has made it difficult to extrapolate findings, make generalised conclusions and create firm clinical guidelines around their use. (Refer to the TGA website for more information.)
A number of systematic reviews and guidelines on prescribing exist. A recent review of the evidence in the European Journal of Internal Medicine suggests medicinal cannabis products may be useful for chronic pain in adults, chemotherapy-induced nausea and vomiting and spasticity associated with multiple sclerosis, and assist with secondary sleep disturbances.
As medicinal cannabis products are considered unapproved drugs in Australia, they can only be accessed through the TGA Special Access Scheme or Authorised Prescriber Scheme.
The application process for a medicinal cannabis permit is onerous, lengthy and difficult for GPs, as it involves obtaining two permits – from the TGA Special Access Scheme and the relevant state poisons department for a schedule 8 permit. This has been a deterrent for GPs to prescribe medicinal cannabis for suitable patients.
The announcement following the recent Council of Australian Governments (COAG) Health Council in Sydney on 13 April – to streamline application and approval process for unregistered medical cannabis products – is encouraging and will hopefully improve and streamline prescribing for GPs.
In addition, it is necessary to obtain approval by another specialist for the use of medicinal cannabis for each patient prior to an application. This often delays prescribing for patients who may benefit, as these specialists are often booked out for months and may disapprove of its use.
Medicinal cannabis products are considered of low toxicity by the TGA, but are best contraindicated in patients with a history of psychotic disorder, concurrent active mood or anxiety disorder, pregnancy, breastfeeding, planning pregnancy and unstable cardiovascular disease until further research is available. They can also interact with medication, particularly with drugs metabolised by, or inhibit or induce, cytochrome P450 (CYP450) enzymes.
While medicinal cannabis is still experimental and new in Australia, there should be no delay in treatment for unwell patients who are in need, such as those experiencing severe chronic pain not relieved by usual medication, chemotherapy-induced vomiting and nausea, and spasticity associated with multiple sclerosis. It is important to note that the TGA advocates that medicinal cannabis be used as a last resort treatment.
Further clarification is needed in the near future, such as advice that a patient cannot drive while undergoing treatment with medicinal cannabis containing THC, as research has shown a patient may test positive to a random drug test while being treated with medicinal cannabis and will be subject to current laws that prohibit driving under the influence of cannabis.
There is a need for more research and it is encouraging that institutions such as the University of Sydney and University of Western Sydney are actively researching medicinal cannabis products.
The RACGP believes GPs who hold a Fellowship are recognised as specialists GP. GPs are in an excellent position to safely prescribe medicinal cannabis products, without the need to refer to other specialists for approval. GPs can monitor for risks and side-effects, identify drug interactions, and report adverse events to the TGA.
Just as GPs are well trained to provide prescriptions for drugs of dependency and analgesia for patients when appropriate, the same principles would apply to prescribing medicinal cannabis products.
Access the RACGP’s Medicinal use of cannabis products position statement for more information.
cannabinoid medicinal-cannabis medicinal-cannabis-prescribing
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?