News
More evidence suggests no long-term COVID-19 immunity
A new longitudinal study has found coronavirus antibodies diminish rapidly within three months of peaking.
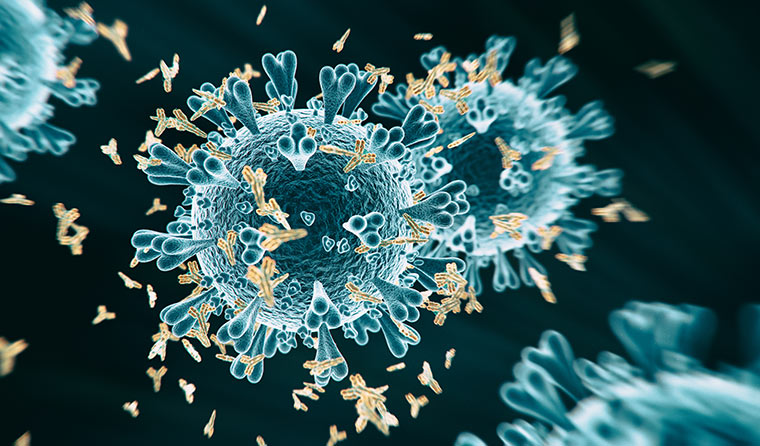 Antibody levels fell rapidly during the study period – and in some cases became undetectable.
Antibody levels fell rapidly during the study period – and in some cases became undetectable.
The research, which was conducted by King’s College London but is yet to be peer-reviewed, is the first to have monitored antibody levels of such a prolonged length of time.
Blood tests taken from more than 90 patients and healthcare workers during the study period revealed that while 60% of people were able to mount a ‘potent’ antibody response to the virus, only 17% retained the same potency three months later.
Antibody levels fell by as much as 23-fold during this time and in some cases became undetectable.
If proven accurate, the King’s College London study would add more evidence to previous findings from China and Spain that also indicate the body does not produce long-term antibodies against SARS-CoV-2.
The study’s lead author Dr Katie Doores told The Guardian that while people were found to be producing a ‘reasonable’ antibody response to coronavirus, it wanes over a short period of time.
Dr Doores added that the findings may also have potential implications for the pursuit of a long-term vaccine.
‘Depending on how high your peak is, that determines how long the antibodies are staying around,’ she said.
‘Infection tends to give you the best-case scenario for an antibody response, so if your infection is giving you antibody levels that wane in two to three months, the vaccine will potentially do the same thing.
‘People may need boosting and one shot might not be sufficient.’
There are more than 155 different vaccines being developed to try to combat COVID-19, but the vast majority are still conducting pre-clinical trials and so far only four have reached phase 3 large-scale efficacy tests.
One, Ad5-nCoV, has been approved for use by the Chinese military, but data from phase 2 trials which reportedly demonstrated a strong immune response have yet to be released.
Others, such as the University of Oxford’s ChAdOxl nCOV-19, have produced mixed results, while many are only now entering phase 1 human trials focused on safety.
Professor Stuart Tangye, Head of Immunity and Inflammation at the Garvan Institute, previously told newsGP the body’s response to COVID-19 suggests any vaccine-derived immunity may be limited in the same way influenza vaccines are seasonal and need to be boosted each year.
Professor Dale Godfrey, Immunology Theme Leader at the Doherty Institute, said research showing poor natural immunity against COVID-19 does not necessarily mean that a vaccine will also fail to induce quality long-term protection.
‘It’s quite possible that vaccines will be able to do a lot more about inducing a good, potent long-term memory response than the actual infection itself,’ he told newsGP.
‘The virus that causes COVID has inhibitory proteins that shut down a lot of our normal immune processes but vaccines can be designed where only a part of a virus is provided, like part of the spike, while adjuvants – molecules that can really enhance immune responses – can be provided as well.
‘You can tip the balance towards a much stronger immune response without all those virus inhibitory proteins that might be trying to inhibit the immune response.’
Flinders University spin-off Vaxine is one company attempting to harness adjuvants in its efforts to produce a vaccine.
It recently began phase 1 human trials at the Royal Adelaide Hospital (RAH), with Chair and research director Professor Nikolai Petrovsky hopeful the company’s recombinant spike protein approach would help provide long-term protection.
‘The COVAX-19 vaccine was developed from Vaxine’s earlier SARS coronavirus vaccine approach, which combines with Vaxine’s non-inflammatory Advax-CpG55.2 adjuvants,’ he said.
‘Past experience with adenovirus-based vaccines has shown disappointing protection and high toxicity, and DNA and mRNA-type vaccines have their own problems, including being unproven technologies that may still turn out to be poorly scalable or have unexpected side effects.
‘Low immunogenicity of adenovirus, DNA and mRNA technologies in particular could be a major problem when it comes to coronavirus vaccines, where immunity will need to be strong and long-lasting.
‘Most of these vaccine technologies are unable to benefit from adjuvants, which are the key turbochargers that are bolted onto protein-based vaccines to dramatically enhance their effectiveness.’
Regardless of the implications for vaccines, Professor Godfrey said studies showing poor long-term immunity to coronavirus indicate Australia’s approach of containment and suppression – rather than herd immunity – has been the right one.
‘The Sweden approach; I don’t think any immunologist would say that herd immunity without a vaccine is a good idea,’ he said.
‘They’re not even close to the necessary threshold for herd immunity, and even if it was going to be a lasting form of immunity, you have to get to around 66% of the population infected, which means potentially one in 30 people will die,’ he said.
‘We don’t really want that and it would be crazy to try for that. In a situation where you don’t even know if the immune response is going last for more than a year, herd immunity is really something you want to aim for with a vaccine, not with the live infection.
‘The way that Australia and New Zealand are doing it, when you really hit it on the head pretty hard now and try to manage the residual situation is a much better approach.’
Log in below to join the conversation.
coronavirus COVID-19 immunity vaccine
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?