News
No longer a death sentence: Australia making progress in diagnosis and management of HIV
Ahead of World AIDS Day, newsGP spoke with a sexual health expert about the progress in the fight against HIV.
 World AIDS Day aims to raise community awareness and support for those with HIV and AIDS.
World AIDS Day aims to raise community awareness and support for those with HIV and AIDS.
World AIDS Day is held on 1 December each year to raise community awareness of HIV and AIDS, and show support for people living with HIV.
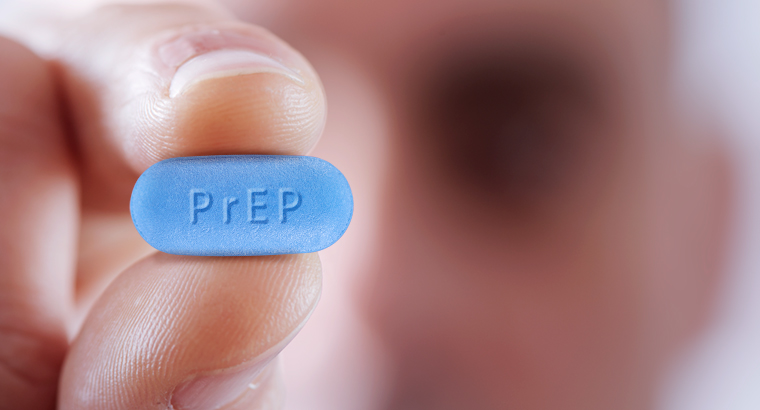
The introduction of pre-exposure prophylaxis (PrEP) to the Pharmaceutical Benefits Scheme (PBS) earlier this year has helped put Australia on the path to becoming one of the first countries in the world to end the transmission of HIV.
In addition, as part its commitment to ending HIV transmission the Federal Government has announced funding for the first HIV self-testing kit, the Atomo Self Test – a single-use rapid finger stick test for the detection of antibodies.
Government funding towards a fifth National Aboriginal and Torres Strait Islander Blood Borne Viruses and Sexually Transmitted Infections Strategy: 2018–2022 is also underway to support closing the gap between Aboriginal and Torres Strait Islander people and non-Indigenous Australians’ health outcomes.
Speaking at Parliament House this week, Labor Senator Penny Wong said Australia is leading the way in tackling HIV and AIDS.
‘As a result of the great work of governments, health professionals, and many others working with the LGBTIQ community ... we are now living in an era where HIV is no longer a death sentence, and we can dare to hope for its elimination,’ Senator Wong said.
‘Diagnosis and treatment need to be supported by community education if progress is to be made.
‘Australia has succeeded because we have proceeded on the basis of inclusion, non-judgement, and we have also tackled prejudice and discrimination along the way.’
Sexual health physician Dr Vincent Cornelisse told newsGP that the introduction of PrEP has been a ‘game-changer’, with Australia seeing a very rapid uptake of the drug.
‘We have been prescribing PrEP [at my clinic] since 2014, initially as part of clinical trials, and now as routine care for people who are at risk of HIV,’ Dr Cornelisse said.
‘Since then we have seen a massive reduction in HIV diagnoses.
‘PrEP has also provided an incentive for people to engage with a GP on a regular basis and for many people this has resulted in other health benefits, such as accessing mental health care, vaccinations, smoking cessation, improved cardiovascular risk and regular sexual health screening.’
 The introduction of PrEP has seen a considerable reduction in HIV diagnoses in Australia.
The introduction of PrEP has seen a considerable reduction in HIV diagnoses in Australia.
Engagement with GPs can also contribute to reducing the number of late diagnoses by offering HIV testing to anyone who may be at risk, a practise Dr Cornelisse believes is not being followed enough.
‘Many people who are at risk of HIV don’t attend specialised sexual health services, and many of these people may not realise that they are at risk of HIV,’ he said.
‘This means they are often diagnosed late, hence they are more likely to develop HIV-related health problems, such as opportunistic infections and cancers.’
Dr Cornelisse identifies the importance of GPs asking routine questions about HIV risk factors to all of their patients by taking a sexual history. Risk factors include male-to-male sex, sex in high-risk countries, a history of sexually transmissible infections and injecting drug use.
There are two main biomedical approaches GPs can use for HIV prevention and management, which assist GPs in their important public health role, according to Dr Cornelisse.
‘One is PrEP – medication by people who don’t have HIV to protect themselves,’ he said.
‘The other is treatment as prevention [TasP], the flip-side of this coin – people who are diagnosed with HIV who are on HIV treatment and have fully suppressed their viral load, cannot transmit HIV to their sexual partners,’ Dr Cornelisse said.
‘In order for TasP to be an effective public health strategy, GPs need to try to diagnose everyone who has HIV to be able to offer them treatment and prevent further transmission.
‘So the effectiveness of this strategy is dependent on people getting tested for HIV.’
Routine screening for HIV and biomedical advances such as PrEP and TasP have proved valuable to the successful progress of reducing and managing HIV diagnoses. This year alone, Queensland has de-listing AIDS as a notifiable disease, new cases of HIV in Victoria are down 22%, and new cases of HIV in Western Australia are at a 10-year low.
However, Dr Cornelisse believes we still have a way to go.
‘[Despite] a significant drop in HIV diagnoses in certain parts of the community, there is currently a danger that some people in Australia are being left behind in this PrEP revolution,’ he said.
Among those being ‘left behind’ are people without Medicare cards who often find it difficult to access PrEP and, according to Dr Cornelisse, there has been a recent increase in HIV diagnoses in overseas-born young gay men.
‘There has also been an increase in HIV diagnoses in Aboriginal and Torres Strait Islander people compared to non-Indigenous Australians, and there is still quite low awareness of PrEP in the general community in Australia, with an increase in HIV diagnoses among heterosexuals in Australia,’ he said.
‘These disparities highlight that GPs can play a very important role in this space by identifying which of their patients are at risk of HIV, offering HIV testing, and offering PrEP.
‘If we are to eliminate HIV transmission, we need to find a way to similarly engage with those parts of the Australian community that are currently not accessing HIV testing and PrEP – GPs are perfectly positioned to help foster such engagement.’
Dr Cornelisse believes the patient–doctor relationship is instrumental to achieving the goal of eliminating HIV in Australia.
‘HIV rates are decreasing rapidly among Australian men who have sex with men, and we should celebrate this as a success that was achieved by close collaboration between doctors, health departments and, most importantly, the gay community,’ he said.
AIDS HIV PREP world AIDS day
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?