News
Poll suggests 93% of GPs have not been offered respirator fit-testing
GPs in NSW and Victorian hotspots are being giving access to PPE from the National Medical Stockpile. But with few practices offering fit-testing, how protected are GPs?
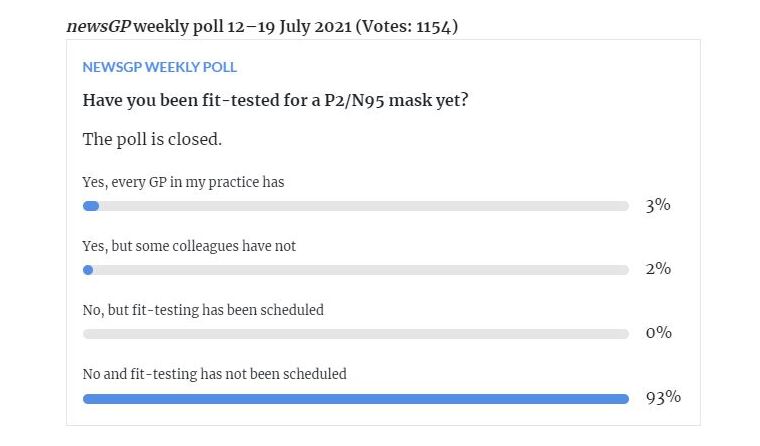
 Out of 1154 respondents to the newsGP weekly poll, 93% said they had not been fit-tested and neither had it been scheduled.
Out of 1154 respondents to the newsGP weekly poll, 93% said they had not been fit-tested and neither had it been scheduled.
The Federal Government has extended its PPE support to GPs in Victorian hotspots, with an initial allocation from the National Medical Stockpile of up to:
- 725,000 surgical masks
- 725,000 N95 masks
- 175,000 pairs of gloves
- 175,000 gowns
- 175,000 goggles.
GPs can request a package of PPE through five PHNs, including North Western Melbourne, Eastern Melbourne, South Eastern Melbourne, Western Victoria and Gippsland.
RACGP Victoria Chair Dr Anita Muñoz welcomed the Government’s offer of PPE, saying that if general practice is to continue to see patients face-to-face during the current outbreak, they need support.
‘Particularly as there are
increasing reports of patients that are presenting into general practice for respiratory symptoms,’ she told
newsGP.
‘If we want GPs to be seeing patients with respiratory illness where there is a risk that that illness will be COVID, understand that GPs themselves have their own risks and their own health conditions to manage.
‘They deserve the same protection as any other healthcare workers – and that protection should be offered by the health system that the GPs are working to support.’
It was
last month that the Infection Control Expert Group (ICEG) updated its
PPE guidelines for healthcare workers, stating that P2/N95 respirators should be worn instead of a surgical mask if there is a ‘likely high risk of transmission’, and that fit-testing should be completed before use.
However,
a poll run by newsGP from 12–19 July found just 5% of the 1154 respondents have been fit-tested, 2% of whom said their colleagues had yet to undergo the process.
Conversely, 93% said they have not been fit-tested – nor has it been scheduled.
Dr Muñoz said the findings are not surprising given that practices, at a state-level, have largely only been supplied with surgical masks.
‘Really the evidence is that fit-testing becomes important if you are treating known positive patients in a hospital environment, for example, or if you are going to generate aerosols with the work that you’re doing,’ she said.
‘In fact, we’re asked to stand down aerosol generating procedures when there are significant outbreaks, like suspending spirometry, for example, in clinic. So that is a logical explanation for that data.’
However, a pre-print study published on
medRxiv on Monday has added to evidence that SARS-CoV-2 ‘can be aerosolised in the absence of coughing, sneezing, and aerosol-generating medical procedures’.
With COVID outbreaks resulting in lockdowns in NSW, Victoria and now South Australia, and a number of general practices listed as exposure sites, Sydney GP and RACGP Expert Committee – Quality Care (REC–QC) member, Dr Michael Tam, says the poll’s findings are ‘concerning’.
‘It really does mean that there is a very substantial risk to general practice if things get out of hand,’ he told
newsGP.
‘Last year the assumption was that it was still just droplet [transmission] and droplet-type protections. But now we know that that’s probably not enough, particularly with the Delta variant.
‘Without the fit-testing, N95s are still better than nothing, but it’s chancy. For it to be demonstratively effective – and it would be the standard in other industries – if you’re going to be using a respirator … it does really need to be fit-tested.’
In contrast to other parts of the world, where GPs are overrepresented in COVID cases, Dr Tam says general practice in Australia thus far has been ‘very lucky’, attributing the low infection rates among doctors to a fast transition to telehealth and the establishment of respiratory clinics.
But he says the current outbreaks around the country are a reminder that a possible risk is always there.
‘At the moment, it’s not too bad; it’s one practice here, one practice there, one pharmacy here, one pharmacy there. But in a setting where we have a major outbreak, this could potentially cripple primary care,’ Dr Tam said.
‘And in Australia, we haven’t had a very strong approach of ensuring a PPE policy in general practice should things go disastrously, and I think it is a concern.
‘Even the distribution of masks; if it’s just one mask, it’s not useful if it doesn’t fit your face.’
Research conducted last year found a substantial proportion of Australian healthcare workers may not pass initial fit-testing, with women of Asian descent
particularly vulnerable.
‘There needs to be a strategy that really responds to and accepts the notion that a substantial number of individuals working in health will need access to airborne protections and that will be access to a range of masks and also to the testing facility so that they can be fit-tested,’ Dr Tam said.
‘If an outbreak suddenly occurs, things can go pear-shaped really quickly. That’s not the time to be trying to organise your sources of PPE and trying to get fit-testing done.’
While Dr Muñoz believes governments should offer general practice the same protections as other healthcare workers, she thinks more needs to be done to hold patients who knowingly withhold information about their respiratory symptoms during the triage process to account.
‘People are deceiving GPs, which is really a questionable thing to do and a really unethical thing to do. But it’s very difficult to know whether we should then be encouraging every single GP and all of the staff in general practice to use much more expensive N95 masks for the handful of cases we’ve seen in the community where those patients are putting the clinics at risk,’ she said.
‘It’s really not a simple question to answer when you think of the huge volume of staff in general practice at work every single day, changing masks twice a day.
‘In an ideal world, we would have the very best of everything all the time. But we’ve also got to pay for a huge number of other components of our public health response.
‘Really, there needs to be a call for the public to contribute to the solution and perhaps suggest that placing healthcare workers and healthcare environments in jeopardy, knowingly, is something that people need to be made responsible for. I think that we need to look at that as an option, rather than accepting that people are going to behave that way.’
The Department of Health was contacted for comment, but did not reply before publication.
Log in below to join the conversation.
COVID-19 fit-testing N95 pandemic PPE
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?