News
PPE taskforce to address urgent shortage concerns in Victoria
The taskforce is designed to provide a coordinated central approach to addressing concerns regarding the supply, demand and usage of PPE.
 The taskforce brings together key stakeholders from across the health sector to work with the Federal Government, manufacturers, hospitals and universities to ensure an adequate PPE supply.
The taskforce brings together key stakeholders from across the health sector to work with the Federal Government, manufacturers, hospitals and universities to ensure an adequate PPE supply.
Victoria’s Department of Health and Human Services (DHHS) has responded to continued concerns over lack of personal protective equipment (PPE) in the fight against coronavirus by establishing a new taskforce dedicated to ensuring PPE is readily available across the state’s health sector.
Headed by Safer Care Victoria Chief Medical Officer Professor Andrew Wilson, the taskforce is designed to provide a coordinated central approach to addressing concerns regarding the supply, demand and usage of PPE.
It brings together key stakeholders from across the health sector, including the RACGP, all of whom are working together with the Federal Government, local manufacturers, hospitals and universities to ensure an adequate supply.
‘This will help us to ensure all healthcare workers in our public health system continue to have access to adequate PPE, so they can protect themselves while doing their very important job – saving lives,’ Professor Wilson told newsGP.
‘Working in healthcare settings is a risk and we are grateful to all our health workforce for stepping up and caring for all Victorians during this coronavirus pandemic.’
Two of the GPs involved are specifically looking into a solution for primary care: Dr Hung The Nguyen, Clinical Advisor and Executive Member of Safer Care Victoria, is a member of the taskforce committee; and RACGP Victoria Council member Dr Bernard Shiu, who will be advising the taskforce.
‘We just can’t get enough PPE to cater for the need. Setting up this taskforce, the aim is to solve that problem,’ Dr Shiu told newsGP.
He said the taskforce would also provide clear information on what PPE should be worn and when, in order to avoid unnecessary use of masks, gowns and goggles.
‘We need to have a clear protocol to follow and we need to have good reasoning why certain PPE is going to hospitals and certain PPE is going to different types of general practice,’ Dr Shiu said.
‘Obviously some of general practices will have greater need. It really depends; it’s a very fluid situation. So we need to move swiftly and then adjust our protocol accordingly.’
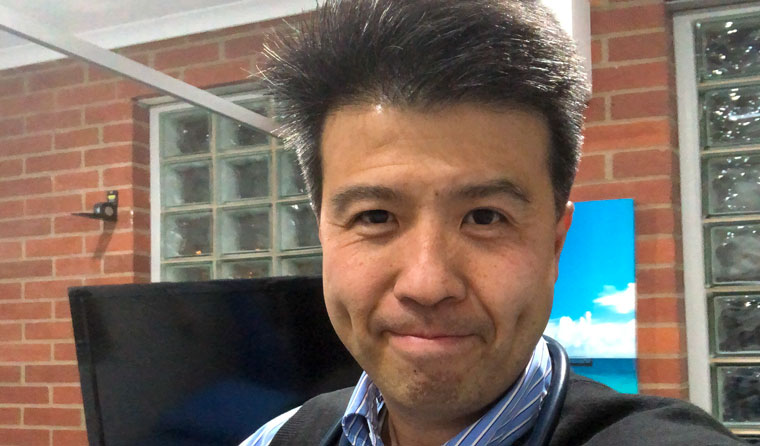
RACGP Victoria member Dr Bernard Shiu is advising a news taskforce dedicated to ensuring PPE is readily available across the health sector.
Lack of PPE has been a mounting concern since the coronavirus outbreak commenced, with GPs and other healthcare workers fearing for their health and safety.
Close to 4500 people signed an open letter demanding state and federal governments urgently provide more PPE, The Age reported.
Federal Health Minister Greg Hunt last week announced more than 11 million masks would be distributed to healthcare workers from Wednesday 8 April , 2.3 million of which would go to Primary Health Networks.
Dr Shiu said it is not yet clear from which stockpiles the millions of masks will be sourced, adding that the news DHHS taskforce would be seeking greater transparency.
‘We want to be clear in terms of stock take; what we actually have in the Victorian stockpile and how much of those federal stockpiles we can actually get access to,’ he said.
Chair of RACGP Victoria Dr Cameron Loy praised the DHHS for listening to the concerns of GPs and showing an understanding.
‘I’m told that some of the supply chain issues are about to be resolved and, for that, well done Victorian Government – you’ve listened to the problems in the health workforce, you’ve understood them and you’re launching a solution to fix that,’ Dr Loy told newsGP.
‘Professor Wilson has sought two general practitioners to be on that committee, so there are GPs who can give real on-the-ground advice as to what’s actually happening out there, and that’s great. That’s what we need.’
When it comes to PPE, Dr Loy says, Australia was ‘caught short’ as a nation.
‘I don’t think we were prepared enough with our medical stockpiles to withstand an event like we’re currently going through. As a result, what we’ve seen is an incredible shortage of PPE,’ Dr Loy said.
‘I counted my PPE this morning. We have two gowns – that’s it.’
‘We've had lots of promises of PPE, but it's still yet to really materialise in general practices and for that matter, significantly in hospitals as well.’
Dr Loy called this situation ‘completely unreasonable’ and believes there is ‘no obligation for GPs to place themselves at risk to do their job’.
A total of 157 healthcare workers have tested positive to COVID-19 in Victoria, according to figures from the DHHS.
Clinics with dwindling reserves of PPE face the possibility of closure, which could place further strain on hospitals.
Many practices have reported taking matters into their own hands, pooling funds to order from manufacturers directly, while others have been using raincoats as gowns, and contemplating the 3D printing of masks.
‘I think that shows a lot of ingenuity within our general practice community,’ Dr Loy said.
‘But it shouldn’t be happening. We should actually have access to PPE.
‘I’m hopeful that that’s the way this committee continues to work – find the problem, get a quick practical solution that gets the job done.’
The RACGP has more information on coronavirus available on its website.
Log in below to join the conversation.
coronavirus COVID-19 PPE taskforce Victoria
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?