News
Progress made on long COVID diagnostic
Australian researchers have made a tool they hope will eventually allow GPs to predict a patient’s likelihood of developing the condition.
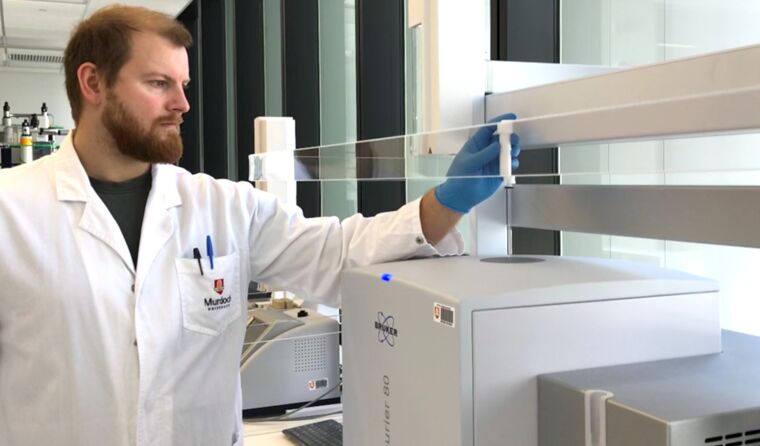 Murdoch University researchers have been using nuclear magnetic resonance to identify molecular biomarkers for COVID. (Image: Murdoch University)
Murdoch University researchers have been using nuclear magnetic resonance to identify molecular biomarkers for COVID. (Image: Murdoch University)
Current estimates suggest around one in every five people diagnosed with COVID still experience symptoms after a month, while around 5% have symptoms that linger beyond three months.
And given almost one in two Australians is thought to have contracted the virus so far this year, there is an expectation that GPs will be increasingly called upon to help treat or refer patients to long-COVID clinics.
However, with no current framework or diagnostic tools, researchers from Perth’s Murdoch University say people suffering from the effects of COVID-19 and long COVID present GPs with a ‘major health challenge’.
To help them address the expected growing burden, they have been working on a tool that can identify molecular biomarkers for COVID – without the need to detect the disease itself – and be easily deployed in medical practices across the world, at low cost.
‘We have been working on new COVID and long COVID diagnostics for over two years now, using some of the worlds most advanced analytical equipment for measuring metabolites and lipoproteins in blood plasma,’ Professor Jeremy Nicholson, Director of Murdoch’s Australian National Phenome Centre (ANPC) told newsGP.
‘One of our most powerful tools is Nuclear Magnetic Resonance [NMR] Spectroscopy … [and] recently [a] major NMR manufacturer introduced a new range of very compact NMR spectrometers operating at low field requiring only a permanent magnet.
‘We bought one of these machines and tried to adapt the experiments we do in the research lab to measure some key biomarkers that we discovered for COVID-19, and by careful modification of the conditions we found a virtual complete agreement between the research and “field deployable” small NMR machine for the same inflammatory signals in the same amount of time.’
The technology works by using a specially designed set of radio pulses to extract signals from inflammatory glycoprotein markers and fats bound to lipoproteins that gives a rapid diagnosis in approximately a minute.
Findings from the most recent study into the technology were recently published in analytical chemistry journal, The Analyst, and Professor Nicholson says they represent a translational triumph that will ultimately benefit COVID-19 patients in clinics throughout the world.
‘We think this technology will probably have many other clinical applications in the future and may be of particular value in monitoring some of the residual effects of long COVID in individual patients,’ he said.
‘The next step is the clinical deployment of the technology in a real setting to generate the sort of validation data needed to appropriately license this technology for diagnostic use.’
Meanwhile, ANPC’s Professor Julien Wist believes the technological advancement will have many benefits, including cutting costs.
‘It ticks all the boxes for a successful translational technology: low costs, low maintenance, no specialist required and no need for complex algorithms to understand the data,’ he said.
Should the research continue as planned successful, Professor Wist told newsGP the tool will be used alongside existing technology used to diagnose and treat COVID, like PCR tests.
‘Blood markers are not used yet to predict who will suffer from long-COVID – this is what we are working on – but instead they provide an objective measurement of the process by which the diseased metabolic signature returns to normal,’ he said.
‘They do different things. PCR is a test for the presence of the virus, but does not provide any information about how it affects metabolism at the different stage of the progress of the infection.
‘In contrast, blood markers do not provide a test for the presence of the virus but provide a direct window to observe its effects on the human body. Thus, they are complementary.
‘PCR for instance tells you nothing about long-covid but metabolism does – what type and how bad.’
And while there is still a ‘long journey ahead’ before the prototype becomes available for clinicians, Professor Wist says it provides hope for the future.
‘The problem is that there is nothing out there that can detect a problem [long COVID] that is and will affect millions,’ he said.
‘There is not instant translation for any new medical technology … [but] those markers were first discovered in 2020 using extremely expensive spectrometers, and less than two years later they are observed and quantified using a benchtop device in less than a minute.
‘These benchtop diagnostic devices have the potential to effectively deliver personalised healthcare in the future. For that to happen we need to be able to measure more biochemical markers.
‘This paper shows a possible way to achieve this goal.’
Log in below to join the conversation.
diagnostic long COVID
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?