News
Rapid uptake of PrEP linked to declining condom use
Experts have told newsGP the findings from a new study should not make GPs reluctant to prescribe the HIV-prevention medication.
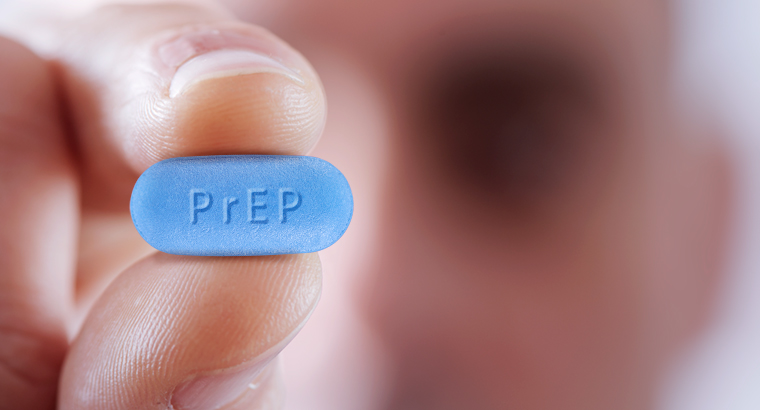 PrEP is said to be is 99% effective at blocking HIV transmission.
PrEP is said to be is 99% effective at blocking HIV transmission.
A major Lancet study has found that the rapid uptake of HIV-prevention medication pre-exposure prophylaxis (PrEP) has come in tandem with declining condom use.
There are concerns that other sexually transmissible infections (STIs) may rise as a result, even though condom use has been falling since 1996.
The study of 17,000 men who have sex with men in NSW and Victoria found that the number of HIV-negative men using PrEP rose from 2% to 24% in the four years to 2017.
Over that period, consistent use of condoms dropped from 46% to 31%.
PrEP became available on the Pharmaceutical Benefits Scheme (PBS) in April this year.
But the Lancet study’s lead author, University of New South Wales’ Professor Martin Holt, warns that the findings should not be interpreted as a call for practitioners to back away from prescribing PrEP.
‘We expected to see a rapid rise in PrEP, and we did, so that was positive. It’s been really successful and demand is really high,’ he told newsGP. ‘There have been no infections amongst people who successfully adhered to the regimen. They’re protected from HIV – it’s quite extraordinary.
‘But we were hoping that condom use would be sustained at a higher level than it was.
‘Gay and bisexual men are much more concerned around HIV than other STIs, and that’s reasonable because most STIs are treatable. We should not put people off PrEP because of STI concerns.
‘There has been enormous effort expended in Australia to make PrEP accessible and on the Pharmaceutical Benefits Scheme and we’re seeing rapid pace of change. I’m really hopeful that will lead to a dramatic decline in [HIV] notifications, because people [on PrEP] are amazingly well protected against HIV.’
‘We have the tools now to stop people getting HIV. It’s an extraordinary chance to get HIV on the eradication pathway in Australia.’
Professor Holt said that what appeared to be happening is a rapid shift in sexual practices. While condoms remain the most common strategy for safe casual sex, the uptake of PrEP means that sexual partners are increasingly basing their risk management on the fact one of them is using PrEP.
‘We are really encouraging men to choose one of the growing prevention options rather than relying on other people,’ he said.
Professor Holt said there is a great opportunity now for GPs to find people, particularly in the gay and bisexual community, who were not using condoms and have a discussion as to whether PrEP is a good option to manage their risk.
He said that a major side benefit of the popularity of PrEP is that many men who have sex with men are getting full sexual health checks at the recommended rate of four times a year when they come to get a new three-month script for the medication.
‘For the first time, we are seeing this huge cohort of HIV-negative gay and bisexual men who are having screening at the recommended guidelines,’ Professor Holt said. ‘So PrEP is a way to engage people in the recommended sexual healthcare, and it allows us to diagnose other STIs much more quickly.
‘This is a really good thing for GPs, to say that when you go on PrEP, we really recommend getting tested quarterly for STIs.’
Melbourne GP and sexual health specialist Dr George Forgan-Smith told newsGP that the new study does not represent bad news.
‘PrEP, when taken every day, is 99% effective at blocking HIV transmission compared to condoms, which are 70%,’ he said. ‘Are we honestly saying we should be promoting a technology that’s less effective at blocking HIV?’
He said that the trend away from condoms is long-running.
‘The condom-only message is failing,’ he said. ‘That’s why a technology like PrEP is so important.’
But he said that condoms would remain an important part of sexual health.
‘We know that other STIs such as gonorrhea, chlamydia and syphilis are reduced by using condoms, but not eliminated. So from a GP perspective, we do need to encourage people to use condoms,’ he said.
Dr Forgan-Smith said he is concerned that some people who are not on PrEP might be choosing not to use condoms if their sexual partner is taking PrEP.
‘We need to encourage people to stop putting control of their sexual health into other peoples’ hands. We need to encourage people to be self-sufficient and 100% in control of their sexual health,’ he said.
‘We need to be open and honest with patients around what their risks are and help them come to a decision.’
Dr Forgan-Smith has seen many patients who are traditionally reluctant to use condoms who have benefitted from PrEP.
‘These people were already not using condoms. So what we’re saying is we acknowledge that and that PrEP is protection against nasty stuff like HIV.’
Dr Forgan-Smith said there remains a good deal of uncertainty among GPs over how to prescribe PrEP and who it would benefit.
‘I see at least two patients a day referred to me by doctors who decline to prescribe it for their patients, either because they don’t know how to or they’re not willing to do it,’ he said.
Dr Forgan-Smith will be presenting an introduction to PrEP at the RACGP’s annual conference, GP18, on the Gold Coast in October.
A new training resource for doctors on PrEP has recently been published by the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM).
condoms HIV HIV-prevention PrEP preventive-health sexual-health
newsGP weekly poll
As a GP, would you benefit from further education about identifying and supporting patients impacted by intimate partner violence?