News
Research shows medicinal cannabis ‘boom’ in Australia
More than 248,000 prescriptions have been approved over the past five years – 85% of which have been given out since January 2020.
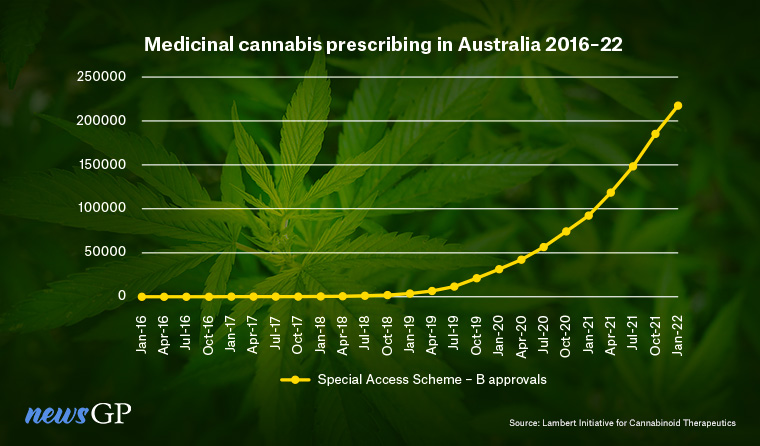 The vast majority of medicinal cannabis prescriptions have been issued via the Special Access Scheme – Category B.
The vast majority of medicinal cannabis prescriptions have been issued via the Special Access Scheme – Category B.
The first in-depth study of Australia’s medicinal cannabis program, which began in 2016, shows it is not only being prescribed more often, but also for increasingly various conditions.
According to data taken from the Therapeutic Goods Administration (TGA), prescriptions have been issued for more than 140 different conditions, in particular pain, anxiety and sleep disorders – despite limited evidence regarding the drug’s effectiveness for treating these ailments.
For Associate Professor Vicki Kotsirilos, Australia’s first authorised GP prescriber of medicinal cannabis and a co-author of the research, the top reasons for prescriptions are not surprising.
‘Pain, anxiety and sleep issues are often interconnected – chronic pain can also cause mental health and sleep issues,’ she said.
However, Associate Professor Kotsirilos told newsGP not enough is known about why Australia has experienced such dramatic growth in the number of medicinal cannabis prescriptions being issued to patients.
‘We need to do more research on why there has been a boom in prescribing by doctors,’ she said.
‘Is it more interest among prescribers, is it patient demand or something else?’
The largest shift has been seen in Queensland, where the normalised rate of growth of Special Access Scheme – Category B (SAS–B) approvals ‘far outnumbers all other states and territories’, the research states.
Likewise, SAS–B approvals increased markedly for flower products during 2020–2021, as did approvals involving younger age groups (18–31 years old), male patients, and non-CBD (cannabidiol) dominant products.
Many of the prescriptions among this cohort were given for anxiety, despite the current evidence base for medicinal cannabis use being limited to only a few studies investigating CBD-dominant products, rather than products that contain psychoactive THC (tetrahydrocannabinol).
‘Historically, the effects of THC have been described as anxiety-inducing, although this may depend on dose size and other factors,’ senior author Dr Elizabeth Cairns said.

Associate Professor Vicki Kotsirilos, Australia’s first authorised GP prescriber of medicinal cannabis and a co-author of the research.
Aside from major trends, the size of the dataset also allowed the researchers to find prescribing patterns in small, but significant, populations that otherwise might have been overlooked.
‘Apart from the link between anxiety and flower products, we found other interesting associations, for example, prescriptions of topical CBD for convulsions,’ Dr Cairns said.
‘This usage has not been extensively explored.’
However, one limitation of the study is that the data does not include information on patient outcomes.
‘Unfortunately, we just don’t know if these treatments were effective for these patients, but this data highlights where we can focus our attention next – to do focused studies and/or clinical trials,’ Dr Cairns said.
‘There is a clear, unmet need for effective drug treatments across a variety of conditions that may be being helped with medicinal cannabis.
‘For example, it could be worth conducting high-quality clinical trials on the use of flower products for anxiety, and that is certainly something that the Lambert Initiative [for Cannabinoid Therapeutics] and its collaborators may look to do in future.’
Such research could also inform the use of medicinal cannabis for pain relief, which comprised 61% of all SAS–B approvals recorded during the study period despite the Australian Faculty of Pain Medicine suggesting not to prescribe medicinal cannabis for this purpose.
Although Associate Professor Kotsirilos prescribes medicinal cannabis for pain, she says this should only be done as a last resort, after more evidence-based behavioural and drug therapies, such as counselling, exercise and deep breathing, have failed or are shown to be of limited clinical benefit.
‘There is a need for better education to ensure GPs are well equipped to advise patients when it’s appropriate and the type of medicinal cannabis, if appropriate,’ she said.
‘More education is also needed around risks and the precautions that need to be taken, to ensure doctors are prescribing to patients safely.’
Log in below to join the conversation.
anxiety medicinal cannabis pain sleep TGA
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?