News
Masks for people in coronavirus hotspots
REPUBLISHED: With Victoria recording 363 more cases on Sunday, masks are now mandatory for residents in Metropolitan Melbourne and the Mitchell Shire.
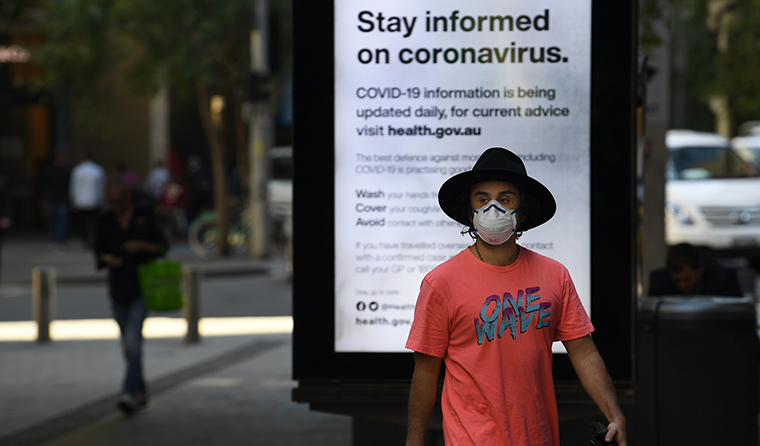 Some leading epidemiologists have advocated for more widespread use of masks. (Image: AAP)
Some leading epidemiologists have advocated for more widespread use of masks. (Image: AAP)
NOTE: This article was first published on 9 July, before Victorian Premier Daniel Andrews declared masks mandatory for residents in Metropolitan Melbourne and the Mitchell Shire.
Victoria’s COVID-19 spike and the World Health Organization’s (WHO) recent admission that coronavirus may spread via aerosols in certain settings has generated renewed interest in the use of masks in Australia.
Leading epidemiologists, such as UNSW global biosecurity expert Professor Raina Macintyre and WHO advisor Professor Mary-Louise McLaws, have advocated for more widespread use of masks, as has the Australian Medical Association.
GPs including Dr Lorraine Baker and the former member for Wentworth Dr Kerryn Phelps have also been vocal supporters of increased mask use and called on Victorian Health Minister Jenny Mikakos to change public health advice in an effort to stem community transmission of coronavirus.
‘I’m asking the Government to counsel people to wear protective re-usable masks for everyone’s protection, and as a sign of solidarity with the sick and those doing it tough because of the virus,’ Dr Baker said.
The Australian Health Protection Principle Committee (AHPPC) has consistently indicated such a blanket approach is not necessary, especially as the evidence supporting airborne infection is still limited.
However, in the wake of Melbourne’s mounting number of cases, Australian Deputy Chief Medical Officer Dr Nick Coatsworth recently responded to questions regarding mask use by encouraging people to use them in certain circumstances.
‘The primary protection to stop this virus from getting from one person to another is, has always been, and always will be, distance between one individual and another,’ he said.
‘[But] in areas of increasing community transmission, where social distancing cannot be performed, masks should be considered.
‘With regard to the rest of Australia and whether vulnerable people should wear masks … [where] there is no community transmission, that widespread community mask use, it remains the position of the AHPPC that that is not indicated.’
This position has led the AHPPC to be accused of lagging behind guidance issued by other public health organisations, such as the WHO and the US Centers for Disease Control and Prevention. But the Chair of Australia’s Infection Control Expert Group, Professor Lyn Gilbert, told newsGP this is not the case.
‘What we have said is that use of masks is not recommended in circumstances in which community transmission is low or negligible, because the chance of unexpectedly encountering an infected person is negligible,’ she said.
‘This has been and still is the situation in most of Australia – even early in the outbreak, when most cases were in returning travellers and their contacts. We always said that the recommendations would change if the circumstances changed, as they now have in Melbourne.
‘We still warn that a mask is not a substitute for other precautions, but suggest that [it] is reasonable to use a mask and/or face shield in situations where community transmission is occurring and physical distancing cannot be maintained.’
Professor Gilbert said the main value of using a mask is to protect others if the wearer is unwittingly infected but asymptomatic, because if a person has symptoms they should not be out in the community.
‘For people who are vulnerable, such as the elderly or those with chronic disease risk, they are probably better off wearing a face shield [with or without a mask] because the eyes are also a potential source of infection via droplets,’ Professor Gilbert said.
However, Professor Macintyre believes the theory that SARS-CoV-2 is spread by droplets and contact only is ‘speculation’ and ‘not based on any good evidence’.
‘There is more evidence supporting face mask use in the community than hand hygiene, including in randomised controlled trials which compare both interventions directly,’ she wrote in the April edition of the Journal of Travel Medicine.
‘It is inconsistent to advocate hand hygiene as a sound principle but not masks.’
Professor Macintyre also cites a recent Lancet study that found face masks reduce the risk of infection with viruses such as SARS-CoV-2 by 67% if a disposable surgical mask is used, and up to 95% if specialist N95 masks are worn.
‘Modelling shows that even a modestly effective mask that delivers just a 20% reduction in viral transmission can successfully flatten the COVID-19 curve. Masks have a double benefit, stopping infected people spreading the virus and protecting uninfected people from catching it,’ she wrote in a recent op-ed.
‘Given the possibility this coronavirus can also be spread by people without symptoms or even people who have already left the room, handwashing and physical distancing may not be enough.
‘We need every tool at our disposal, and that includes masks.’
Log in below to join the conversation.
coronavirus COVID-19 masks social distancing
newsGP weekly poll
Would it affect your prescribing if proven obesity management medications were added to the PBS?