News
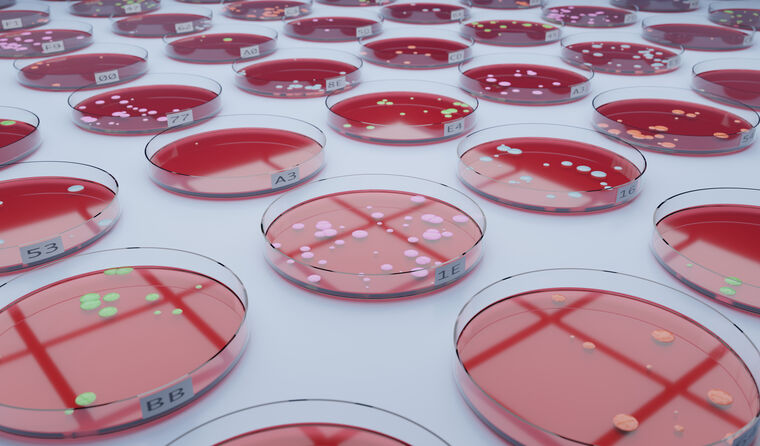
‘Superbugs’ causing great harm in Australian children: Study
Almost 10% of kids with a bloodstream infection are infected with a multi-drug resistant organism, in a ‘serious and growing problem’.
 Bacterial antimicrobial resistance was directly responsible for 1.27 million global deaths and contributed to 4.95 million deaths in 2019.
Bacterial antimicrobial resistance was directly responsible for 1.27 million global deaths and contributed to 4.95 million deaths in 2019.
Groundbreaking new research has revealed Australian children are getting sicker from hard-to-treat infections, with one expert saying there is an urgent need for GPs to practice mindful prescribing.
The landmark study found 9.4% of children admitted to hospital with bacteraemia are infected with multi-drug resistant (MDR) organisms.
Nationwide, researchers singled out staphylococcus aureus, known as golden staph or S. aureus, as the most common bacteria found in children aged one year old or above.
They also discovered significant differences in pathogens and antimicrobial resistance across geographic areas, as well as variances between organisms in children compared with adults.
It is now hoped the first-of-its-kind study will be used as a benchmark for future research in the field, as well as calling urgent changes to the way antibiotic are prescribed and used.
Professor Mark Morgan, Chair of RACGP Expert Committee – Quality Care, told newsGP the research is yet another reminder that while many GPs are considered in their prescribing, much more can be done.
‘This is important research that demonstrates how antibiotic resistant “superbugs” are already causing great harm,’ he said.
‘Community use of antibiotics has reduced gradually over the last decade but there is still a great deal of over-use compared to best-practice guidelines, particularly for acute respiratory infections.
‘It is vital that antimicrobial stewardship is practised consistently across all sectors of healthcare.’
The study ran between January 2000 and December 2021 and saw 38 Australian laboratories collect blood culture samples from children admitted to hospital with bacteraemia.
Recorded infections included both community and hospital-acquired infections, with neonates experiencing the highest mortality rates.
Specifically, researchers found that almost half of S. aureus isolates from the Northern Territory were methicillin-resistance, followed by Western Australia where it sat at 19%.
While rates of enterobacterales infections were highest in New South Wales and Victoria respectively, with Victoria recording the highest rates of MDR.
Almost three-quarters of the 170 enterococcus spp. reported were E. faecalis, and half were from patients less than one year old.
The report’s lead author and infectious diseases epidemiologist Anita Williams said antimicrobial resistance amongst children is a ‘serious and growing problem’ that is likely to cause many infection-related hospital admissions and deaths in the future.
‘The study gives us valuable insight into how antimicrobial resistance varies according to geographic location, which can help guide localised treatment recommendations,’ she said.
‘But it also tells us that no matter the location – all children are at risk of resistant infections.’
The World Health Organization (WHO) has labelled antimicrobial resistance as one of the top global public health and development threats, saying ‘the world faces an antibiotics pipeline and access crisis’.
It estimates that bacterial antimicrobial resistance was directly responsible for 1.27 million global deaths and contributed to 4.95 million deaths in 2019.
‘The misuse and overuse of antimicrobials in humans, animals and plants are the main drivers in the development of drug-resistant pathogens,’ the WHO said.
Professor Morgan said both clinicians and the public can have an ‘exaggerated impression of the benefits of antibiotics’ in reducing the severity, duration and complications of infections.
‘Every day in general practice we are balancing the need to treat infections promptly, particularly recognising the early signs of sepsis with the need to avoid over-use of antibiotics,’ he said.
‘This all occurs in the context of maintaining therapeutic relationships, safety netting, and managing patient expectations. It is challenging and rewarding work that relies on years of training and experience.’
In 2023, 22 million antimicrobial prescriptions were supplied in Australia, which is 17% lower than 2019 and 24% lower than 2015.
But Professor Morgan said there is an urgent need for additional resources to help GPs practice antimicrobial stewardship.
‘As a GP, I would find it useful if the Therapeutic Guidelines were regularly updated with regional resistance patterns so that I could make informed choices about the best antibiotic to use once I’ve made the clinical decision that an antibiotic is indicated,’ he said.
‘It would be even more useful if trusted computer decision support pop up provided the information at the appropriate time during a consultation.’
Log in below to join the conversation.
antibiotics antimicrobial resistance bacteria multi-drug resistant organism
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?