News
‘Urgently needed’ guidance issued for healthcare COVID exposure sites
A new matrix developed by the Department of Health allows clinics to assess their level of risk without having to furlough entire practice teams.
 In the most common scenarios, where general practice staff are fully vaccinated and wearing adequate PPE, exposure to COVID-19 is unlikely to result in quarantine.
In the most common scenarios, where general practice staff are fully vaccinated and wearing adequate PPE, exposure to COVID-19 is unlikely to result in quarantine.
The prospect of a COVID-positive patient unknowingly walking through the doors is a front-of-mind concern for most general practices – especially as community transmission grows and Australia edges closer to easing restrictions.
But fears of having to shut down and furlough entire practice teams have been allayed thanks to new guidance issued for workers in healthcare settings by the Federal Department of Health (DoH) on Friday.
Designed to support safe decision-making, the 13-page document includes a framework practices can use to help determine whether the exposure is low-risk (casual contact) or moderate- to high-risk (primary contact), along with subsequent steps to take.
The risk assessment matrix takes a number of factors into consideration, including details of the confirmed case, type of exposure, location and duration of contact, as well as mitigation strategies such as vaccination status, personal protective equipment (PPE) and ventilation.
The guidance comes after months of frustration, wherein practices unknowingly exposed to COVID-19 were left with no option but to close or run on a skeleton staff, despite strict adherence to protective measures.
RACGP Victoria Chair Dr Anita Muñoz, who helped inform state guidance for Victorian practices, told newsGP it will make ‘a big difference’ to GPs.
‘The furloughing rules have been very, very challenging … and causing a huge concern to GPs because they want to deliver services to their patients, but they’ve also got to run a private business,’ she said.
‘So this was very urgently needed, and we definitely understood that.’
A common scenario for general practice that is deemed medium risk is indoor contact with a patient that lasts between 1–15 minutes with a distance of at least 1.5 metres and the patient wearing either a surgical or cloth mask.
If the staff member is fully vaccinated and wearing a surgical mask and eye protection, the scenario would be deemed low risk and the worker classed a casual contact, allowing them to continue to work while undergoing surveillance testing, including a PCR test on day one, two and five.
However, in the instance that the staff member is unvaccinated, the risk level increases to moderate. As a primary contact, they would be required to leave work as soon as possible to get tested and quarantine until day five test results are available.
If baseline and day five tests are negative, the staff member can return to work with an exemption letter from the DoH. Further surveillance testing must also be carried out with PCR tests on days seven and nine, or daily rapid antigen tests or saliva tests on each working day, with a day 13 clearance test also required.
During this time, the staff member is also required to wear an N95 respirator at all times on site and should not share staff-only spaces or work across different sites.
However, with N95 respirators required in a number of scenarios included in the matrix to avoid being classed a close contact, access to PPE and fit testing remains an ongoing concern.
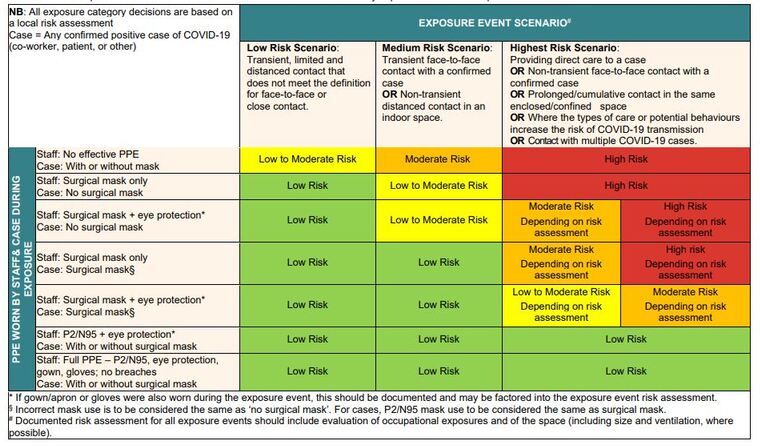
The exposure risk matrix released by the DoH for fully vaccinated workers in health care settings.
Dr Muñoz said this was acknowledged by the state health department during her discussions, and assured that efforts are underway to secure supply.
‘The department listened to that very carefully and of course recognise that that could be one of the limiting factors for GPs in terms of accessing N95 masks, which we know are more expensive than surgical masks,’ she said.
‘So in addition to publishing this [guidance], Louise Galloway at the Department of Health has wanted to make it clear that she is taking the request for N95 support for GPs to our federal colleagues.’
Last year, frontline GPs were told Federal Government-supplied PPE from the National Medical Stockpile was only a ‘fallback’ option and that they should instead largely rely on commercial supplies.
Dr Muñoz said she has been involved in weekly meetings with the state health department, relaying member feedback, but noted the diverse nature of general practice had made developing guidance particularly challenging.
‘From the beginning, furloughing whole general practices was seen as a really urgent matter that needed to be resolved,’ she said.
‘But unfortunately, like everything in this pandemic, it’s incredibly complex and the department needed to make sure that their guidance was not going to cause unintended consequences.
‘Writing a document that could be applied in all of our various scenarios was quite challenging and it of course requires a lot of support documentation. But that’s now been achieved after a huge effort.’
Victoria is the first state to issue guidance specifically for general practices, and has provided more detail than the national guidance.
As states inch closer to achieving their vaccination targets and New South Wales prepares to significantly ease restrictions on Monday, Dr Muñoz said other states and territories would likely benefit from providing the same level of detail.
‘Having something this well thought out and this clear … I do suspect will make general practices perhaps less skittish about the idea of engaging in medicine in an environment in which there is circulated COVID,’ she said.
‘We may find that other states or other environments haven’t got to this point of thinking in this much depth yet because need has not dictated that they do that.
‘But from the Victorian experience, once there is a need there is a sudden sense of urgency to answer the question. So having access to our work may be a very positive thing for other constituents.’
As well as exposure to COVID-19 in clinical settings, the guidance can be applied to situations where a healthcare worker has become a close contact due to a community-based exposure.
Even if case numbers continue to surge in Victoria, Dr Muñoz said it is unlikely the state’s matrix will change, as it is based on whether an individual case is positive or not. However, a new variant of concern could see advice change.
‘I hope that we never have to have a conversation about a new and different strain. But in the current environment and what we predict to be the future, I would expect that this document will serve us into the future,’ she said.
‘It’s an excellent example of the great relationship developing between RACGP Victoria and the Department of Health, which means that we can work closely on projects like this, particularly in an urgent manner, to deliver changes in general practice.
‘After a lot of hard work, in particular on the part of Deputy Chief Health Officer Suman Majumdar, I’m very, very pleased to get this into the hands of GPs.’
Log in below to join the conversation.
COVID-19 exposure site eye protection fully vaccinated N95 masks PPE
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?