News
Who is seeking pharmacotherapy treatment for opioid dependence?
Annual data examines who, where and why on a ‘snapshot day’ in 2020, and how treatment has progressed.
 Around 61% of authorised prescribers are authorised to prescribe more than one type of pharmacotherapy treatment for opioid dependence.
Around 61% of authorised prescribers are authorised to prescribe more than one type of pharmacotherapy treatment for opioid dependence.
Male, aged 44, living in Victoria or New South Wales, taking methadone for heroin dependence.
That is the average profile of a person in Australia receiving pharmacotherapy treatment for opioid dependence, according to the latest report from the Australian Institute of Health and Welfare (AIHW).
It used information from the National Opioid Pharmacotherapy Statistics Annual Data (NOPSAD) collection, which revealed that in 2020 on a snapshot day, 53,316 people received pharmacotherapy treatment for their opioid dependence at 3084 dosing points across Australia.
Around two in three (67%) of these people were male – a proportion that has remained stable since 2011 – while both males and females in the 40–49 age group had the highest rate of treatment, with 44 years the median age.
Between 2019 and last year, there was a 4.7% increase in the number of people receiving treatment, the largest increase over the past decade.
Dr Paul Grinzi, a GP with a special interest in addiction medicine, told newsGP there are a number of factors that have contributed to the increased number of people accessing treatment.
‘Over the past decade there has been an enormous shift from patients using heroin to more commonly now using prescription opioids,’ he said.
‘These patients are in our waiting and consulting rooms. They have access to us and if we conduct an alcohol and other drugs [AOD] assessment, we will detect our patients who have lost control of their opioid use.
‘There is also greater acceptance and awareness of opioid-use disorder being a treatable condition.’
Dr Grinzi, who is also an educator on the RACGP’s AOD GP Education Program, said ‘thousands’ of GPs have already accessed the program.
‘There’s clearly a thirst for upskilling in this clinical area,’ he said.
The increase in people accessing treatment for opioid dependence was largely driven by growth in New South Wales and Victoria, with AIHW data indicating that the shift in Victoria may be in part due to the April 2020 implementation of the SafeScript initiative, part of a move to nationwide real-time prescription monitoring.
For NSW, the increase could be attributed to the introduction of buprenorphine.
‘South Australia, Victoria and NSW have made prescribing sublingual buprenorphine/naloxone much easier, with all GPs now able to prescribe to their patients, sometimes with limits on numbers,’ Dr Grinzi said.
‘NSW and Victoria have the highest population numbers and both have made prescribing buprenorphine/naloxone easier for all prescribers. Both states have also ramped up the accessible training and education for prescribers over the past few years.
‘Real-time prescription monitoring systems such as SafeScript are being rolled out nationally, albeit slower than many of us would like; so this should certainly assist us in identifying those patients who have lost control of their opioid use and require additional help.’
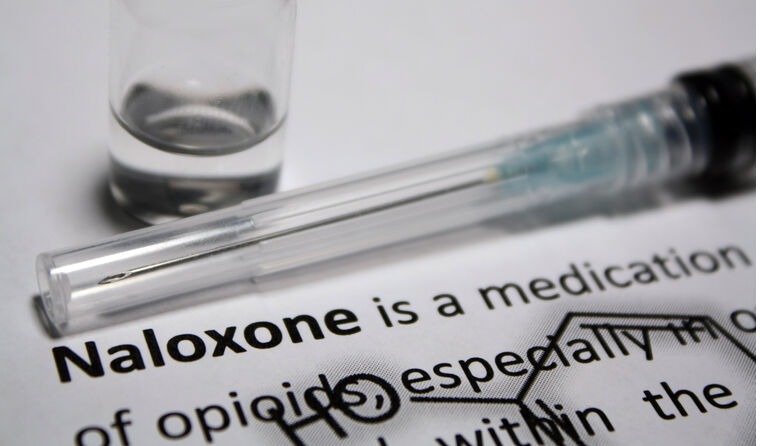
Methadone, buprenorphine, buprenorphine-naloxone and buprenorphine long-acting injection (LAI) are the four medications registered for long-term treatment for opioid dependency in Australia.
Methadone continued to be the most commonly prescribed pharmacotherapy treatment, with 58% of people treated on the snapshot day in 2020, a decrease from 69% in 2011.
This was followed by buprenorphine-naloxone which rose from 18% in 2011 to 21%, and sublingual buprenorphine which rose from 14% in 2011 to 19%.
Buprenorphine LAI is reported for the first time in the NOPSAD 2020 collection given it has only been available since 2019, with 2.4% of people accessing the treatment in 2020.
Dr Grinzi hailed the introduction of buprenorphine-naloxone and LAI formulations in reducing harm and overcoming barriers to accessing treatment.
‘The buprenorphine-naloxone formulation has significantly reduced the dangerous practise of injecting buprenorphine, previously seen with the sublingual buprenorphine-only formulation, which is now rarely prescribed or indicated,’ he said.
But he said the benefits of take-home naloxone are yet to be fully recognised.
‘Take-home naloxone is sadly under-prescribed across our nation, especially for patients at higher risk of unintended overdose, such as patients with opioid disorder, those taking more than 100 mg oral morphine equivalent per day, those co-prescribed benzodiazepines, and patients who have a previous history of overdose,’ he said.
‘If we frame take-home naloxone in the same way we frame the EpiPen for anaphylaxis – prescribed to help treat a life-threatening condition, with the hope it’ll never need to be used – GPs can open up the discussion and increase our prescribing of the PBS-subsidised medication.’
On snapshot day in 2020, the AIHW found there were 3422 authorised prescribers of opioid pharmacotherapy medicine, a 15% increase since 2016.
Of these prescribers, around 61% were authorised to prescribe more than one type of treatment.
While 20% were authorised to prescribe buprenorphine-naloxone only, 9.7% were authorised to prescribe buprenorphine only, and 9.4% authorised to prescribe methadone only.
The private sector, such as general practice clinics, hosted the majority (82%) of these prescribers, with the remainder working in the public sector (13%), correctional facilities (3.7%) or a combination of sectors.
Irrespective of the type of pharmacotherapy treatment, most people (71%) received their pharmacotherapy treatment at a pharmacy.
And that link between GP prescribers and pharmacists is key, according to Dr Grinzi.
‘One of the wonderful parts of prescribing opioid pharmacotherapy is the relationships I’ve developed with community pharmacists,’ he said.
‘The majority of patients will be seeing me frequently for clinical review and their prescriptions and their nominated pharmacists on a daily-weekly basis, depending on stability.
‘The pharmacists have an important role in the treatment of his population and the cross-professional communication and collaboration is essential.’
Log in below to join the conversation.
buprenorphine naloxone opioid addiction pharmacotherapy treatment
newsGP weekly poll
Would it affect your prescribing if proven obesity management medications were added to the PBS?