Feature
Self-collection of HPV samples: A guide for GPs
Dr Lara Roeske writes for newsGP about self-collected samples, a key aspect of the renewed National Cervical Screening Program.
 The self-collection sampling swab should be inserted to the red mark.
The self-collection sampling swab should be inserted to the red mark.
Self-collection is an alternative pathway to overcome barriers some women experience to having a clinician-collected cervical screening test. Australian data has demonstrated that at least 80% of women who develop cervical cancer in Australia are under-screened or never screened. Eligible women can now take the sample themselves and have access to life-saving cervical screening tests.
Self-sampling is available to women at least 30 years of age and who are considered under-screened (four or more years since the last Pap smear), or who have never been screened and who decline a clinician-collected specimen.
Women who are eligible for self-collection will benefit from participation in screening, especially if disease is detected and treated. They will also benefit by being reassured they are at low risk of cervical cancer if oncogenic human papillomavirus (HPV) is not detected.
Key points for GPs
- Self-collection is a vaginal swab taken by a woman for HPV testing
- The sample contains vaginal rather than cervical cells
- The vaginal HPV test is sufficiently accurate and includes partial genotyping for HPV 16 and 18
- There is some loss of sensitivity compared to a clinician-collected sample; however, HPV testing of self-samples is more sensitive than a Pap smear at detecting underlying high-grade cervical lesions and better than no cervical screening test
- Liquid-based cytology (LBC) cannot be performed on the vaginal sample
- Self-sampling must be performed in a healthcare setting under the supervision of a healthcare professional who also offers cervical screening – it is not available as a home-based test or mail-out kit
- The resulting laboratory report will be sent to the practitioner, not the woman
Tips for supporting women to take a vaginal self-sample for HPV
Women who are eligible for self-collection may be more anxious about cervical screening. It is important for GPs to reassure women about the test in a sensitive and culturally appropriate manner.
The below visual guide can also help to explain how the test is done. It may be useful to show the woman the sampling device, describing the soft-tip and indicating they should insert the swab up to the red mark. It can also be helpful to explain that taking the sample should not hurt.
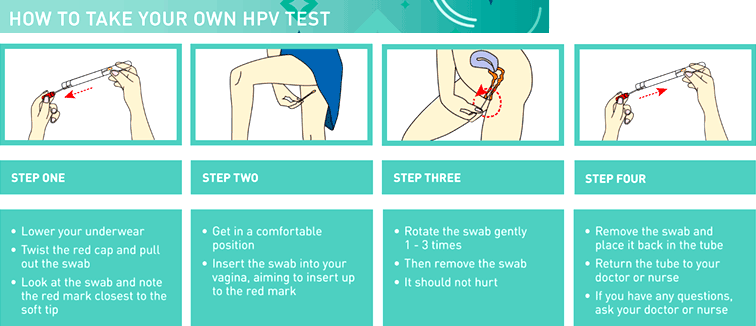 This image is adapted from Garrow SC et al. The diagnosis of chlamydia, gonorrhoea, and trichomonas infections by self-obtained low vaginal swabs in remote northern Australian clinical practice. Sex Transm infect. 2002 Aug. 78 (4) 278-81.
This image is adapted from Garrow SC et al. The diagnosis of chlamydia, gonorrhoea, and trichomonas infections by self-obtained low vaginal swabs in remote northern Australian clinical practice. Sex Transm infect. 2002 Aug. 78 (4) 278-81.
Document the woman’s preferred method of contact and update these details, discuss and document how they will receive test results and what follow-up is required if HPV is detected.
Follow-up of test results
If oncogenic HPV is not detected on a self-collected sample, GPs should explain that the risk of developing cervical cancer is low. They should then tell the woman she will be invited to re-screen in five years (add receive a recall for a cervical screening test in five years) and that a clinician-collected sample will be offered and encouraged at that time. This is because the clinician-collected sample provides the most effective protection against cancer of the cervix.
Additionally, if oncogenic HPV is detected in the clinician-collected (cervical) sample there is no need for a second visit to collect cells from the cervix for reflex (LBC). This also allows visualisation of the cervix at the time of sampling.
If oncogenic HPV is detected on a self-collected sample, these women can be contacted by the practice to arrange a follow-up visit. At this visit, the GP can refer for colposcopy for women with oncogenic HPV (16 or 18) detected. This should not be delayed. The cervical sample for reflex LBC will be obtained at the time of colposcopy.
For women with oncogenic HPV (not 16 or 18) detected, GPs can collect a sample from the cervix for reflex LBC. It is important to explain to the woman that the cytology result will guide further management.
If the reflex LBC test result is negative, low-grade squamous intraepithelial lesion (LSIL) or possible LSIL, explain that she must return in 12 months for a follow-up HPV test. A clinician-collected sample will be taken from the cervix at that visit.
If the LBC test result is high-grade squamous lesion (HSIL), possible HSIL or any glandular abnormality, tell the woman further investigation is required and a referral to a specialist for colposcopy will be organised at the earliest opportunity, preferably within eight weeks.
Self-collection should not be offered to:
- pregnant women
- women with possible symptoms of cervical cancer (bleeding, pain or discharge)
- women under the age of 30
- women who have had a hysterectomy and a past history of HSIL of the cervix.
Further resources
Support self-collection in general practice, including a visual guide –
www.vcspathology.org.au/practitioners/self-sampling-resources
Self-collection pilot study and publications relevant to the National Cervical Screening Program –
www.vcs.org.au//publications/scientific
National guidelines on self-collected vaginal samples –
https://wiki.cancer.org.au/australia/Clinical_question:Self-collected_vaginal_samples
‘How to take your own HPV test’ is provided by VCS Pathology and reproduced with permission.
HPV-test National-Cervical-Screening-Program self-collection self-sampling
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?