News
Bullying reported by over a third of medical trainees
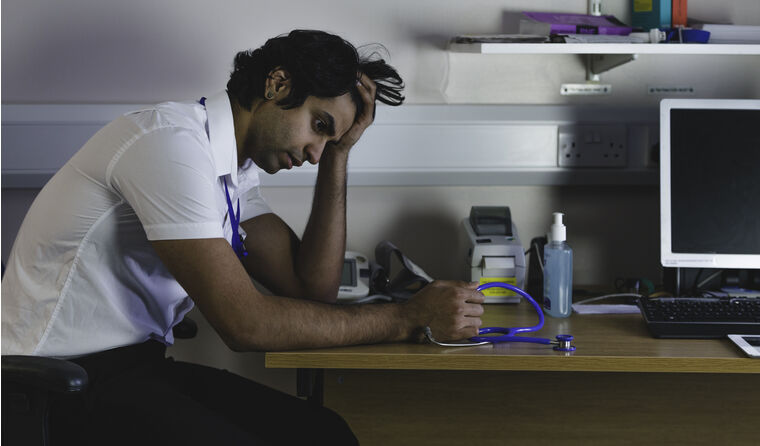
Many of those who experience bullying, discrimination or harassment say it has adverse impacts on their training.
 The results of the medical trainee survey will inform policy recommendations to Australia’s National Medical Workforce Strategy.
The results of the medical trainee survey will inform policy recommendations to Australia’s National Medical Workforce Strategy.
Workplace culture continues to be a serious issue in medical training, results from the latest national Medical Board of Australia (MBA) Medical Training Survey confirm.
The results show little improvement in workplace culture, with issues such as bullying, harassment and discrimination still being experienced, especially among Aboriginal and Torres Strait Islander trainees.
More than 21,000 medical trainees – more than half of the current cohort – participated in the 2021 profession-wide survey, designed to address feedback and identify key issues to inform policy recommendations to Australia’s National Medical Workforce Strategy.
While all aspects of the quality of supervision for trainees have improved since 2020, with 80% of respondents recommending their training program and current workplace, 35% experienced or witnessed bullying, harassment and/or discrimination, including racism.
Those who were impacted suggest senior medical staff are the most culpable, with 51% saying they experienced bullying, harassment and/or discrimination from this source, while 54% had witnessed senior medical colleagues engaging in that type of behaviour.
These figures represent no improvement on previous years, further highlighting the serious and ongoing issues that often lead to stress, burnout, depression and even suicide among junior doctors.
Around 38% of trainees who experienced bullying, discrimination and/or harassment reported in the survey that it had ‘moderate’ or ‘major’ adverse impacts on their training.
For Aboriginal and Torres Strait Islander trainees, those figures are worse. Fifty-two per cent experienced some form of bullying, discrimination and/or harassment, with 49% reporting a ‘moderate’ or ‘major’ impact on their training.
MBA Chair Dr Anne Tonkin said the survey results provide important insights into medical workplace culture, the quality of training and areas for improvement.
‘Year on year, [survey] results are showing there’s a lot going well in medical training in Australia,’ she said.
‘But some small changes in 2021, which may relate to the impact of the pandemic, warrant close attention in the years ahead.’
Dr Jacinta Power is an Aboriginal woman and recent James Cook University (JCU) medical graduate, who now works for JCU General Practice Training.
Although she did not experience bullying, harassment or discrimination throughout her general practice training, she was certainly aware of the issues.
‘My experiences were very mixed on clinical placements,’ Dr Power told newsGP.
‘Some rotations we had lovely and caring consultants and others couldn’t care less if you were there or not, and you felt like a fly on the wall that couldn’t move for fear of getting in the way.’
Dr Power attributes her positive training experiences to supportive medical educators who delivered extra exam training, in addition to the routine teaching provided, as well as three ‘amazing’ clinical placements.
‘I had passionate supervisors willing to teach and that also valued a healthy work−life balance for me having a young family,’ she said.
In addition, the support Dr Power received from the Indigenous GP Registrars Network had a positive impact on her training experience.
‘[This] provided a culturally safe space to draw strength from our mob who often were going through similar life and study issues,’ she said.
The importance of a culturally safe space is also highlighted in the results from the Medical Training Survey, which reveals that Aboriginal and Torres Strait Islander trainees are 1.5 times more likely to experience and/or witness bullying, harassment and/or discrimination than non-Indigenous Australian trainees.
‘Disturbingly, there is a significant and unacceptable difference in the incidence of these issues reported by Aboriginal and Torres Strait Islander doctors in training,’ Dr Tonkin said.
‘Racism in healthcare is never acceptable and we all have to do better.’
These findings represent little progress from the survey’s previous years, and a 2017 report on the Australian Indigenous Doctors’ Association member survey on bullying, racism and lateral violence also confirms that closing healthcare disparities – a key Closing the Gap strategy − is unlikely to be achieved without addressing systemic racism.
Part of this strategy is strengthening the healthcare workforce with more Aboriginal and Torres Strait Islander people, for which the RACGP has long advocated for.
The 2020 General Practice: Health of the Nation report there was a 55% increase in Aboriginal and Torres Strait Islander students pursuing a career in medicine compared to the previous three years, with those numbers expected to rise.
Dr Power said that although she did not personally face bullying, harassment or discrimination during her general practice training, her hospital training was a different experience altogether.
‘I had a very different experience in my hospital training where there was a strong undercurrent of competitiveness that would be acted out as bullying,’ she said.
‘I still get a sick feeling in my stomach thinking about this.
‘For an Aboriginal doctor who was already on an uphill journey to get to where they are today, this magnified that feeling of imposter syndrome.
‘As a trainee doctor, another area that was hard to cope with, was the number of racist comments made, often subconsciously and from multiple staff in the hospital, not often directed towards me but towards our mob who were patients.
‘This was a daily occurrence in the hospital training and it would be a matter of picking what battles to fight and which ones to not stand up for, because it was just too tiring to be that person to always say something.’
However, Dr Power says the survey lends insight into how improvement can be made to medical workplace culture, particularly for Aboriginal and Torres Strait Islander people.
‘Learning from what things went right for those who had great experiences [and] drawing on values and teaching from those leaders and teachers who inspire and have positive feedback from their trainees [would be invaluable],’ she said.
‘For Aboriginal and Torres Strait Islander medical trainees, there is still a long way to go with understanding what cultural safety is for our mob. This is slowly changing, which is great, but there is still a long way to go.
‘Cultural education needs to be incorporated for all involved in healthcare right through to the level of administration.’
Log in below to join the conversation.
Aboriginal and Torres Strait Islander bullying GPs in training junior doctors medical training survey
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?