News
Changes likely for GP-generated summaries in My Health Record
Shared health summaries are set for a shake-up after the head of the Australian Digital Health Agency flagged the need for a broad modernisation of the technology underpinning My Health Record.
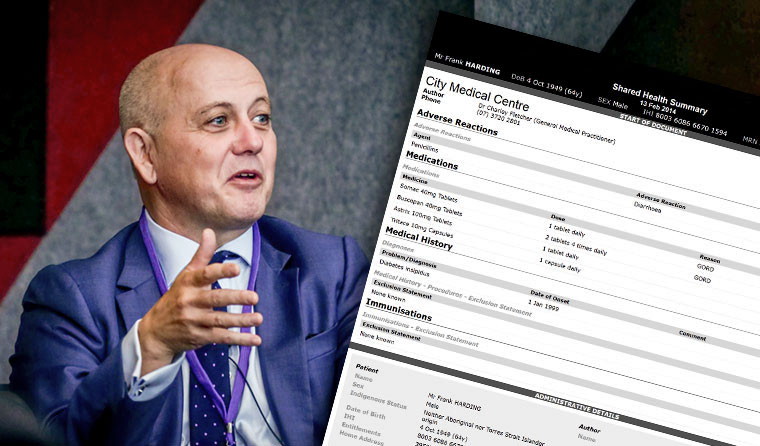 ‘While [it was built with] good intentions, we’re still operating a system that was designed a decade ago for a very different world,’ ADHA chief Tim Kelsey said of My Health Record.
‘While [it was built with] good intentions, we’re still operating a system that was designed a decade ago for a very different world,’ ADHA chief Tim Kelsey said of My Health Record.
Speaking at the RACGP’s eHealth forum last week, Tim Kelsey said there is an opportunity to ‘modernise My Health Record’s infrastructure’.
Mr Kelsey was speaking in response to a question from prominent RACGP digital health advocate Dr Nathan Pinskier, who had asked whether it was now time to reassess the ‘value proposition’ of shared health summaries.
‘We designed shared health summaries around 10 years ago. My feeling is we need to go back and have a look at why we’re asking GPs to upload shared health summaries, how it fits into their workflow, what the value proposition is, and whether there’s a better way of doing it,’ Dr Pinskier said at the forum.
‘Now’s a great time to revisit this. Do we need shared health summaries, or is there a better way of extracting data, as in other parts of the world?’
Mr Kelsey said he ‘completely agreed,’ pointing to the Australian Digital Health Head Agency’s (ADHA’s) push this year to move forward on interoperability more broadly in digital health.
‘What we haven’t worked out yet is the governmental appetite for interoperability, [but] I believe it will be very positive. That will give us the mandate to have that much broader conversation … [o]ver how we design My Health Record to be fit for the future,’ Mr Kelsey said.
‘While [it was built with] good intentions, we’re still operating a system that was designed a decade ago for a very different world.’
The My Health Record program began in 2012 under a different name, the Personally Controlled Electronic Health Record.
Speaking after the event, Dr Pinskier told newsGP shared health summaries in their current form are not delivering for GPs.
He said Mr Kelsey holds a similar view.
‘If you ask 100 GPs about electronic prescriptions, almost all would say it’s wonderful – because it happens in the background, as a by-product of our work. If you did the same for shared health summaries, you’d get a handful,’ Dr Pinskier said.
‘We don’t want to make more work for GPs; we want to consolidate existing workflows.
‘GPs don’t see them as part of their routine workflow. They don’t derive an immediate benefit. It creates additional work and sends information to a government repository for a future use for an unknown provider in unknown circumstances.
‘It’s got a really unclear clinical use case.’

‘Do we need shared health summaries, or is there a better way of extracting data, as in other parts of the world?’ Dr Nathan Pinskier asked at the recent RACGP eHealth forum.
Dr Pinskier said a revised health summary useful to GPs could borrow from models in other countries where data is directly extracted from existing clinical software.
In this model, only important information that had changed between two points in time would be uploaded, meaning My Health Record would act as a living document rather than generating new documents with much repeated information after every consultation.
‘If you made it semi-automated, where new medications or allergies were automatically identified and pushed up to the national record, it would take away complexity and angst,’ Dr Pinskier said.
Nine in 10 Australians had a My Health Record created for them in February. That was when the My Health Record opt-out period ended, following months of at times tense debate around the privacy and security of health data uploaded to the Government’s system.
My Health Record – intended as a central repository for Australians’ health information – is seeing significant growth in data uploading, with a huge uptake from pharmacists and imaging services.
More than 3.1 million shared health summaries have now been uploaded to My Health Record, mainly by GPs, while more than 32 million prescriptions and 16 million pathology reports have been uploaded.
But GPs have had mixed views to date, with some reporting it is now proving its clinical use, while others are yet to be convinced. One reason for that may be that healthcare-organisation uptake varies state by state.
An issue for some GPs is the fact that the GP-generated summaries require additional clicks, rather than being seamlessly produced from the clinical notes a GP inputs during every consultation.
Mr Kelsey said at the eHealth forum that he and his team would be discussing new technology options for My Health Record in coming months, with a focus on newer interoperability standards like Fast Healthcare Interoperability Resources (FHIR).
‘That will resolve into a much more modern service,’ he said.
The focus on FHIR comes after the creator of the standard, Grahame Grieve, called for a major revision of My Health Record’s underlying technology, which he said was state of the art in 2007.
In a submission to the Senate inquiry, Mr Grieve said that while initial designs for My Health Record were more distributed, it is ‘now, unfortunately, a centralised national database of static summary documents …. [t]his was an inevitable consequence of the technical standards used at the time, but now constrains the use, extensibility and therefore the value of the system’.
digital health ehealth interoperability my health record shared health summary
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?