News
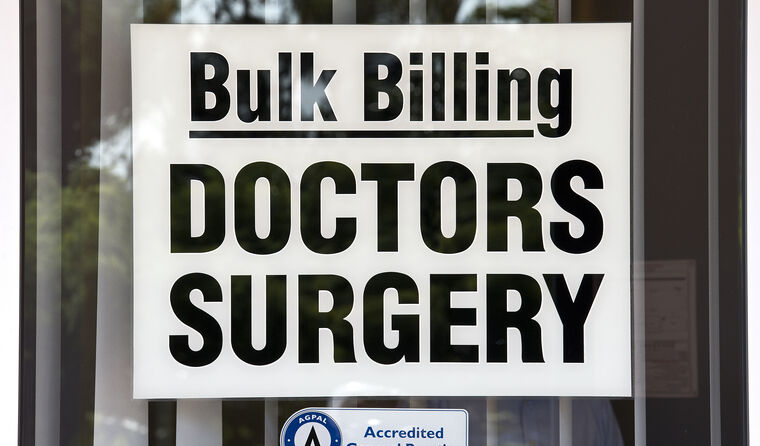
Fall in bulk billing a rising concern for patients
Worries about GP costs are now one of the main issues for patients, with new bulk-billing data indicating that may rise further.
 More than a quarter of survey respondents (26%) said their GP had changed prices, with 88% of them now paying more.
More than a quarter of survey respondents (26%) said their GP had changed prices, with 88% of them now paying more.
The decline in bulk billing, rising costs and health workforce shortages are causing mounting patient concern, a report informed by more than 11,000 consumer responses shows.
The Australian Healthcare Index, a twice-yearly survey produced by the Australian Patients Association and consumer healthcare platform HealthEngine, is designed to provide a snapshot of healthcare from the perspective of patients.
It compares patient experiences across different healthcare areas around the country, including general practice, dentistry, pharmacy, and emergency departments (EDs).
The most pressing concern, according to the 11,405 people surveyed nationwide for the fourth and most recent report last November, is the shortfall in healthcare workers, including GPs and nurses.
Almost half of the respondents (47%) identify that as the highest priority.
Following that, participants were most worried about ED waiting times (42%), with the increasing out-of-pocket costs to see a GP/other doctor identified by a third (33%) of respondents as the next biggest challenge facing healthcare.
Out-of-pocket costs had not featured in the previous report, published in June last year, although patients did raise Medicare cuts as an issue.
‘Cost of living is a major problem in the Australian economy at present,’ said Stephen Mason, the CEO of the Australian Patients Association, in a webinar following the report’s release.
‘We’re finding a lot of people can’t afford all their prescription medication and … a lot of people are concerned about the cost of seeing a GP.
‘It is concerning what the future of bulk billing is, because there’s fewer and fewer clinics offering bulk billing facilities.’
More than a quarter of the people (26%) who responded to the survey said their GP had changed prices, with 88% of them now paying more.
Of those, 53% said they will go to their GP less often, with one in 10 saying they had changed their GP/clinic due to the increased costs.
Meanwhile four in 10 of the people surveyed said they had noticed increased waiting times in the six months leading up to last September.
The study also signalled a widespread lack of popularity for telehealth video consults, with only 16% of patients saying they would prefer to have a video consultation over a telephone consult.
The college has consistently advocated for longer phone consultations to be reinstated, citing concerns over lack of access for the most vulnerable Australians.
Shortly after the release of the Australian Healthcare Index report, the CEO of HealthEngine Dr Marcus Tan raised concerns that the trends highlighted in the report could grow worse, and increase pressure on hospitals.
‘My feeling is the fact that a lot of the out-of-pocket costs at general practice and the diminishing of bulk billing is occurring, we’ll probably see more and more activity happening in public hospital EDs, largely because it is free and there is no out-of-pocket cost,’ he said.
Official figures released last month revealed that out-of-pocket costs have deteriorated further since the Australian Healthcare Index report, with bulk-billing rates shown to have reached their lowest rate in a decade in the final quarter of last year (October to December). The responses for the Healthcare Index Report were gathered last September.
There was a drop of almost 3% in the overall bulk-billing rates for non-referred GP visits, falling from 83.4% in the first quarter of this financial year to 80.5% most recently, its lowest level since 2010–11.
‘GPs can no longer afford to subsidise patient care,’ RACGP President Dr Nicole Higgins previously told newsGP when the most recent MBS figures were released.
‘GPs have simply had enough – many have had to make the difficult decision to move to mixed billing and pass on some of our costs on to patients just to stay afloat.
‘As a patient, I would be asking the Government, “Why haven’t they invested in my Medicare rebate?”
‘I am encouraging my patients to go to their local MP and tell them that this is not good enough. This is the result of successive governments neglecting general practice.’
The Australian Healthcare Index survey also clearly showed the pivotal role of general practice within the health system, with the overwhelming majority of patients (89%) saying they had a regular GP. Of those, more than half (53%) said they would recommend their GP to a friend, a sentiment largely based on the quality of advice and care received.
The majority of patients (64%) said that mental health is the medical condition that needs improved access to support services, followed by cancer (37%) and dementia (28%).
The survey also showed that for non-emergency health concerns, patients are overwhelmingly most likely to seek advice from their GPs – although the results showed significant variation between age groups.
Among younger respondents aged 18–34 years, GPs are at the top of the list with 46%, a figure much lower than for those aged 65 years or older, of whom 72% said they would first go to GPs for advice.
Overall, 58% of respondents said they would go to their GP first, followed by Google (17%), a family member (8%), then pharmacists (7%).
The report also highlighted a consistent decline in the level of personal satisfaction with healthcare in Australia, going down from a rating of 7.8 in March 2021 to 7.1 most recently.
Log in below to join the conversation.
bulk billing healthcare data Medicare patient out-of-pocket costs
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?