News
Saving lives and money: Report provides ‘powerful economic argument’ for primary care funding
New research shows increased investment in preventive health would pay for itself many times over.
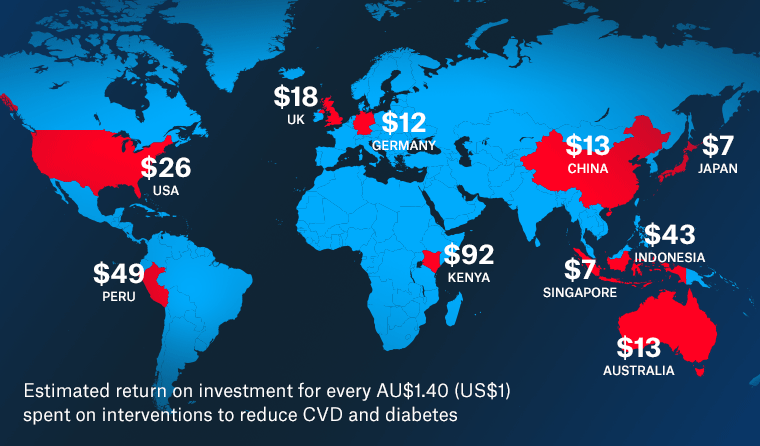 Overall, the 27 countries featured in the report would realise an average return of $28.30 for every $1.40 (US$1) invested in cardiovascular disease and diabetes.
Overall, the 27 countries featured in the report would realise an average return of $28.30 for every $1.40 (US$1) invested in cardiovascular disease and diabetes.
The Victoria University report, commissioned by the US Chamber of Commerce, models the economic returns associated with funding preventive health initiatives aimed at working people aged 40–64.
It estimates that countries would realise an average return of $28.30 (US$20) from productivity gains, lower health costs, and workers’ lives saved for every $1.40 (US$1) they invested in cardiovascular disease (CVD) and diabetes.
Similarly, countries would see an average return of $31.15 (US$22) for every $1.40 invested into anxiety and depression.
‘Increasing rates of chronic disease around the world are having an alarming impact on workforce productivity, global development, and economic opportunity,’ the report states.
‘There is a powerful economic argument for investing more in NCD [non-communicable disease] prevention and treatment so that people can work more productively, thereby reducing social and economic exclusion, and improving the health resilience of the populations.’
Study co-author Professor Bruce Rasmussen told newsGP the research reinforces the importance of primary care investment in preventive health interventions.
‘Preventive programs are the way to go,’ he said.
‘[Current] health expenditures are too skewed towards acute illnesses and a lot can be done about particularly chronic disease by treating early.
‘Part of the reason why we are getting such high benefit–cost ratios is they are just the standard interventions – they don’t cost very much and the drugs that are used are generic.
‘The benefits to these sort of treatments are just so enormous and the costs are modest, so this is why we should get on and do it.’
The analysis, which captures 27 nations from around the globe, uses statistics derived from the World Health Organization’s (WHO) OneHealth Tool.
Based on the report, investment in preventive interventions for CVD and diabetes in Australia would generate comparatively more modest returns of around $12.75 (US$9) for every $1.40 spent. This indicates better existing preventive health programs than some other countries, but also an opportunity for more targeted funding.
Australian general practice attracts a relatively small per-person expenditure in comparison to public hospital funding.
The RACGP has consistently called for greater investment in primary care and Dr Michael Wright, Chair of RACGP Expert Committee – Funding and Health System Reform (REC–FHSR), told newsGP the new report reinforces the college position that investment in chronic disease management saves both lives and money.
‘With most chronic diseases being managed by GPs in the community, this research shows that supporting general practice is a great investment for our economy,’ he said.
‘We need to focus the health system on better managing chronic health conditions, such as diabetes and high blood pressure, and keeping people out of hospital.
‘Doing that not only will keep people healthy, but it’s great for the economy.’
Dr Wright said while most Australians are fortunate to have good health and high standards of living, it also means the impact on the economy can be greater when people are unable to work due to chronic diseases that could have been prevented or managed in the community.
‘We need to encourage people to keep well, and we need to encourage prevention of chronic diseases along with early and better management of them,’ he said.
‘All of this can be done in general practice if it’s better supported to do so.’
Despite the report indicating Australia has a higher burden of disease related to mental health in comparison to the majority of other countries involved in the analysis, the researchers were unable to provide a local benefit–cost ratio due to anomalies in the statistics contained within the OneHealth Tool.
However, Professor Rasmussen said a ‘back of the envelope’ calculation suggests it would be close to the US, which has a similar burden of disease.
‘The economic benefit–cost ratio would be around 16 [ie $16 return on $1 of investment], which is two above where the US is,’ he said.
‘On top of that there would be a social benefit of around two, and that’s based on other similar developed countries.
‘So I think we’re looking at a total benefit–cost ratio for Australia around 18.’
Dr Wright said the research underlines the fact chronic health interventions are not limited to conditions like diabetes and high blood pressure, but also mental health conditions such as anxiety and depression.
‘Those mental health conditions have a major impact on people’s ability to work and they’re also conditions which can be well managed in general practice,’ he said.
‘As a society, we want to keep people as healthy as possible and what this study shows is that doing so will also help improve the productivity of the economy, which is important as we enter the current recession.’

Queensland GP Dr Maria Boulton believes increased mental health presentations since the pandemic mean there is now an even greater need for more funding.
Dr Maria Boulton, a Queensland-based practice owner and member of REC–FHSR, told newsGP the increase in mental health presentations since the pandemic means there is now an even greater need for increased primary care funding.
‘At our clinic, we’ve seen a rise in [mental health] presentations of more than 30%, and there’s also been some data showing a rise in young people presenting with eating disorders post-COVID as well,’ she said.
‘Given the waiting lists to see a psychologist or a psychiatrist, for example, in Brisbane, are three to six months, GPs are having to carry the load for a greater time.
‘There’s going to be a need for further funding in that space, especially for GPs, as 75% of people who have a mental illness present to their GP first.
‘We need to fund longer consultations so we can look after those patients because they’re not a five-minute-medicine job; you actually need to spend quality time with them.’
According to Dr Boulton, the problem is likely to only get worse.
‘People weren’t presenting as much in April or May, for many, many reasons,’ she said. ‘But in the past month or so, we’ve seen lots and lots of people who’ve been previously well [presenting with mental health concerns], or patients whose depression or anxiety was really well controlled, but COVID has caused them to have a recurrence in their symptoms.
‘The burden falls on us because we’re the ones that see them first, as well as the ones that look after them until they get to see a psychologist or a psychiatrist.’
The researchers also believe greater investment in preventive health will be invaluable in a post-COVID world. Aside from the associated health and economic gains, it would likely make future populations more resistant to any future pandemics.
‘Heart conditions, diabetes and COPD [chronic obstructive pulmonary disease] are major factors for the severity of COVID-19,’ the report states. ‘An Italian study revealed that 96% of patients who have died in the hospital from COVID-19 [there] had at least one comorbidity.
‘To achieve long-term success in the fight against COVID-19 and build resiliency going forward, policymakers, clinicians and employers must remain steadfast in their pursuit in addressing the NCD crisis.’
Dr Wright said it is imperative that health authorities continue to encourage patients to remain vigilant in their management of existing chronic disease.
‘We know during COVID many patients have put off having their chronic conditions managed,’ he said. ‘Now more than ever it’s important that we support general practice to manage this growing burden of chronic disease, so that it doesn’t cause a massive tsunami of disease and unnecessary economic impact.
‘Everything in this report shows how important it is that patients get their chronic diseases managed and that GPs are supported to do so.’
Log in below to join the conversation.
cardiovascular disease diabetes mental health preventive health
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?