News
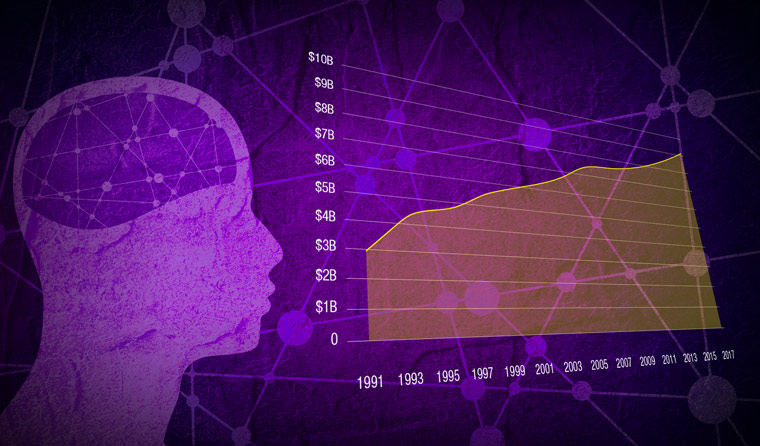
GPs on frontline of $9.1 billion battle
Demand for mental health care continues to grow, with 2.4 million Australians receiving Medicare-subsidised services in 2016–17.
 Of $9.1 billion expenditure on mental health, $5.7 billion was spent on state/territory services, $2.6 billion on public hospital services, and $2.1 billion on community services.
Of $9.1 billion expenditure on mental health, $5.7 billion was spent on state/territory services, $2.6 billion on public hospital services, and $2.1 billion on community services.
This demand translated to $1.2 billion in benefits for Medicare-subsidised mental health-specific services in 2017–18, while an additional $534 million went towards mental health-specific prescriptions under the Pharmaceutical Benefits Scheme (PBS).
Of the $9.1 billion overall expenditure on mental health, or $375 per person, $5.7 billion was spent on state/territory mental health services, while $2.6 billion went towards public hospital services. Community services received $2.1 billion.
GPs were are the forefront of delivering mental health care by providing Medicare-subsidised services to 8.1% of the population in 2016–17, as opposed to 2.7% from psychologists, 2% from clinical psychologists, 1.6% from psychiatrists and 0.4% from allied health professionals.
The statistics, derived from a recently-released Australian Institute of Health and Welfare (AIHW) report, show that the 9.8% of the population that accessed Medicare-subsidised mental health-specific services in 2016–17 had grown from 5.7% in 2008–09.
These statistics also only tell part of the story: they are for services billed against mental health-specific MBS item numbers, which is only a sub-component of GP mental health-related activity.
Overall, approximately 12.4% of GP encounters were mental health-related in 2015–16, an increase from 10.8% in 2007–08.
However, while GPs provide the bulk of subsidised mental health care services in Australia, GP expenditure only comprised $299 million, or 24.1% of total Medicare subsidised mental health-related benefits in 2017–18, compared with $551 million for services provided by psychologists and $358 million for psychiatry.
Contrastingly, GPs accounted for almost three quarters (73.2%, or $392 million) of the expenditure on mental health-related subsidised prescriptions.
According to the 2015–16 data used as part of the report, the prescription, supply or recommendation of medications accounts for 61.6 per 100 problems managed, making it the most common form of GP management of mental health-related issues.
Antidepressants were the most commonly prescribed, recommended or supplied medication (27.8%), followed by anxiolytics (9.8%), and hypnotics and sedatives (9.1%).
Depression, anxiety and sleep disturbance were the most frequent mental health-related problems. Together, they represented 60.8% of all mental health related-problems managed by GPs, and 5.1% of all health problems managed.
Counselling, advice or other clinical treatments were the second most common form of management of mental health-related problems provided by a GP (49.6 per 100 mental health-related problems managed).
People aged 65 and over had the highest rate of mental health-related estimated GP encounters (1198.2 per 1000 population) compared to the general population (749.9), and the rate of encounters was higher for non-Indigenous Australians than for Aboriginal and Torres Strait Islander people (658.6 and 578.7 per 1000 population, respectively).
Referrals were given by GPs at a rate of 18.8 per 100 mental health-related problems managed, with 9.3 sent to psychologists and 2.7 to psychiatrists.
Australian Institute of Health and Welfare government expenditure mental health
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?