Feature
IWD: View from the eye of the COVID storm
From a Canberra general practice to the heart of the COVID-19 response, Dr Stephanie Davis reflects on her career and the challenges for female GPs.
 Dr Stephanie Davis has played a number of important roles in Australia’s response to COVID-19. (Image: Supplied)
Dr Stephanie Davis has played a number of important roles in Australia’s response to COVID-19. (Image: Supplied)
There are few GPs who have as extraordinary a perspective on the global pandemic as Dr Stephanie Davis.
As the rumblings of a mystery virus grew in late 2019, Dr Davis was working part-time as a GP in Canberra.
By February 2020, she had travelled nearly 5200 km to be part of the Australian Medical Assistance Team (AusMAT) on Christmas Island when evacuees from Wuhan began to arrive.
From there, her journey at the heart of the country’s COVID-19 response continued, culminating in an appointment as Deputy Chief Medical Officer (DCMO) last autumn.
Her experience was uniquely well-suited: as well as being a GP, Dr Davis is a Fellow of the Australasian Faculty of Public Health Medicine and has also worked as a senior epidemiologist at the World Health Organization (WHO).
From the outset of the pandemic, she was thrust into a relentless working pattern which she describes as ‘an enormously steep learning curve’.
Due to leave the DCMO post in December, she agreed to carry on until last month to assist the response to the emerging Omicron variant. She says the prospect of leaving at that point made her feel like she would be ‘walking away in the middle of a “resus”’.
While admitting surprise at the level of government bureaucracy she experienced during her time in the role, Dr Davis reflects on her involvement with pride.
‘One of the real highlights was being part of the setup of the general practice respiratory program, which I think was a really fantastic program,’ she told newsGP.
It also challenged any perception of a faceless bureaucracy.
‘The level of goodwill of how much people really wanted it to work, I suppose I hadn’t realised before, the commitment that people within those roles have to try to improve health,’ she said.
During that time, Dr Davis tried to cling on to her clinical work by working a day at the practice – but the workload ultimately interfered.
‘I would be getting home at stupid o’clock ... and it just wasn’t safe or sustainable. I had to give it up, which I really didn’t like doing,’ she said.
‘The practice was under strain … my patients, I really didn’t want to leave them. But it just wasn’t a safe way to practice.’
Having a seat at the table of the COVID-19 response has, however, given Dr Davis a positive sense of general practice’s standing in Australian healthcare.
She believes the status of GPs has been elevated as a result.
‘I don’t think this is just me trying to say something nice, I actually do think there was a greater appreciation of the role general practice plays in the response to public health emergencies,’ Dr Davis said.
‘I don’t think that was well acknowledged before this.’
Going forwards, she believes general practice is likely to be more integral to emergency planning and the implementation of those plans in the future.
‘If you read the previous pandemic plan, which I did at one point … general practice was one line in a 50-page document, which is crazy,’ she said.
‘Again, it’s not due to a lack of goodwill, I think it was a lack of understanding of the role [GPs] have.
‘Having a proper emergency playing out now shows the incredible importance of general practice within any kind of overarching emergency plan.’
While Dr Davis welcomes this shift in attitude, there are other important reforms to general practice she believes need to happen, particularly to address existing gender inequalities.
‘The same structural challenges exist for women in general practices and many other branches of medicine,’ she said.
‘Often training time coincides with having children. I had my baby during training so I’m well aware of the issues with that.’
She would like to see a greater acceptance of part-time work – particularly during training – and is also a strong advocate for workplaces making it easier for men to go part-time and take extended paternity leave.
‘It’s really important for men to have that opportunity, that’s a wonderful thing to be involved in,’ Dr Davis said.
Likewise, Dr Davis believes change is needed with regard to burnout and the greater burden on female GPs in addressing mental health care issues.
‘It’s [about] ensuring that the rebates reward appropriately those kinds of care and the more complex care which is generated by longer appointments,’ she said.
‘That’s a whole of Medicare issue but I think that’s the elephant in the room with pay disparity.’
Dr Davis’ assessment appears to be supported by the GP community as a whole, with nearly two thirds of respondents to a recent newsGP weekly poll identifying increased Medicare remuneration for long consultations as the most pressing change needed in general practice to better serve women.
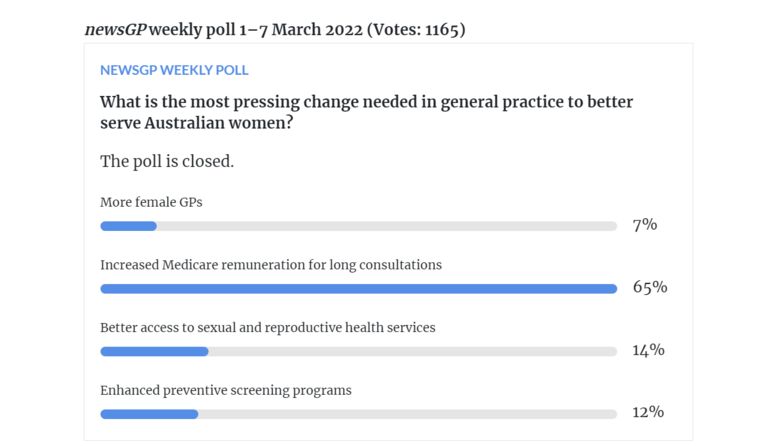
Increased Medicare remuneration was identified as the most pressing change required in general practice to better serve Australian women.
And while she says the all-consuming nature of her work in the past years means she probably is not the right person to advise on work/life balance, Dr Davis does have some thoughts on what has worked for her.
‘I’ve always had a combination of general practice and non-clinical time and I have found that enormously rewarding,’ she said.
‘And just having a little bit of time off, either completely off or not doing something which is still related to medicine but not seeing patients, is a good way of spreading the mental load.
‘But I know not everyone is able to take those opportunities, so it’s really tricky.’
Dr Davis is also passionate about the value of mixing public health expertise and general practice.
‘General practice and public health is such a beautiful combination … that’s where you really make a difference to population outcomes by combining a public health approach and a primary care approach,’ she said.
‘General practitioners are so integral to public health, not just [for the] emergency response, and not just as clinicians, but also because you understand the problems of the community.
‘I would really encourage any general practitioners who are interested in public health to really look at it as another piece of their work, if they can, and look at how they can get involved.’
Now enjoying some time off, Dr Davis says she is excited about returning to the consulting room again.
‘General practice is just an endlessly fascinating endeavour,’ she said. ‘It’s a fantastic career. You never know what’s going to walk through the door.
‘And … patients are just wonderful. I was just decluttering this morning, and I was looking through the stuff I’ve shoved in drawers [since the pandemic began] and I found so many thank you notes and cards from people I’ve seen over the years.
‘There’s just nothing that can make you realise more that you’re doing a good job, and that you are making a difference to people’s lives.
‘What a privilege and opportunity, hey?’
Log in below to join the conversation.
COVID-19 GP International Women's Day public health
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?