News
Major reset to vaccination program: What will it mean for GPs?
GPs have welcomed the National Cabinet’s proposal to revise the vaccine roadmap but say supply issues must be addressed before any major changes are made.
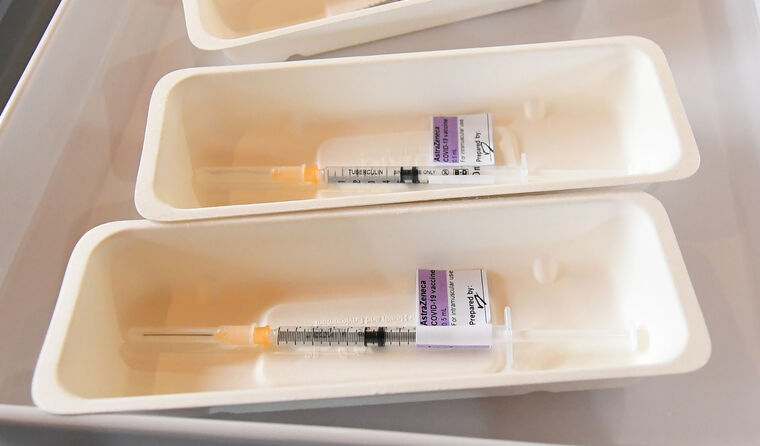 People aged 50–70 could soon become eligible to receive the AstraZeneca COVID vaccine much earlier than planned. (Image: AAP)
People aged 50–70 could soon become eligible to receive the AstraZeneca COVID vaccine much earlier than planned. (Image: AAP)
Australia’s GPs are set to become a more significant part of the country’s vaccine rollout earlier than expected.
Following Monday’s National Cabinet meeting, a proposal was made for people aged 50–70 – previously slated to receive their COVID vaccine from the middle of the year – to become eligible much earlier than planned.
State and territory leaders have agreed to the idea in-principle, and if the policy receives approval on Thursday, these patients will likely soon be able to receive AstraZeneca from a participating general practice or a state-run mass vaccination hub.
The move, which has been labelled a ‘big reset’ for Australia’s COVID-19 vaccination strategy, comes after the Federal Government failed to reach its initial targets and then hit a road bump with AstraZeneca amid concerns over rare blood clots.
Dr Bruce Willett, RACGP Vice-President and Chair of RACGP Queensland, welcomed the prospect of an expansion to the eligibility criteria, but says ongoing supply issues must be ironed out first to meet demand.
‘I think it’s a great thing. The issue for this country is to get us vaccinated so we don’t have to suffer lockdowns and can get our lives back,’ he told newsGP.
‘But I’m not sure what the mass vaccination clinics will achieve at this stage because we’re still supply-limited, rather than manpower-limited, which is the only part where we don’t have a problem.’
While it was projected that local AstraZeneca manufacturer CSL would by now be producing up to one million doses per week out of its Melbourne facility, that weekly number currently sits at around 800,000.
The limited supply to this point has frustrated GPs and practice owners who revised their practice set-up and invested in infrastructure and additional staff so they could play their role in ensuring national targets would be met.
Melbourne GP Dr Shea Wilcox is one such GP.
He set up what is effectively a scaled-down mass vaccination clinic at his East Brunswick practice, with capacity to vaccinate 200 people a day. But he has only been receiving 100 doses a fortnight.
‘First of all, we ran through all our vaccines on the first day,’ Dr Wilcox said. ‘The demand is huge; however, we cannot get the vaccine doses that we need.
‘It’s not a lack of people available to give a dose that’s the issue. There just doesn’t seem to be any vaccine dosages around. It’s frustrating.’
Dr Willett’s practice is in a similar position; five weeks into phase 1b of the rollout, he is still only receiving 100 doses per week.
‘We go through our week’s allocation of vaccines in two hours – that’s how long they last,’ he said.

RACGP Vice-President Dr Bruce Willett says GPs are not being used to their full capacity.
Melbourne GP Dr Mukesh Haikerwal is an advocate of expanding the eligibility criteria, but says GPs need more ‘surety’.
‘What this will mean for general practice is we have a significantly greater chance of doing the job more swiftly because there’s less time determining eligibility or not; people will just be eligible because they’re 50 and over,’ he told newsGP.
‘It does mean we have to have supply of vaccine and it does mean we have to have some surety around this whole process … [and] around indemnity, because I’m hearing in my clinic today that many clinics have stopped vaccinating patients and so they’re sending them off to us.
‘So we just need to bring some surety back into the system – some more comfort to doctors to keep doing this.’
Since GPs came on board on 22 March, they have administered more than half of the 1.6 million doses that have been delivered since the program began in February.
Dr Willett is proud of his GP colleagues and not surprised at their ability and willingness to step up, but says they are not being used to their full capacity.
He believes GPs’ value has been further emphasised since the Australian Technical Advisory Group on Immunisation (ATAGI) changed its recommendation for people under 50, with a preference for the Pfizer vaccine rather than AstraZeneca.
While practices have reported an increase in vaccine hesitancy among older patients, Dr Willett says it has been a particularly significant problem in mass vaccination centres, indicating moves to redirect vaccine supply to general practices would be a better strategy.
‘That shows, of course, the importance of GPs vaccinating their patients because of that level of trust that patients have with their own GP who knows them and their individual health circumstances. So there’s far less reluctance in that circumstance than there is in the mass vaccination clinics,’ he said.
‘We’ve been saying from the beginning that vaccination is core business for general practice – it’s what we do and have done for literally decades, efficiently, quickly and safely.’
But despite the likelihood of phase 2a beginning earlier than expected, National Cabinet maintains that the priority remains to complete phases 1a and 1b, with the Federal Government continuing to finalise the vaccination of aged care residents with Pfizer using an in-reach model.
Melbourne GP Dr Mukesh Haikerwal supports expanding the eligibility criteria.
To cater to population groups under 50, the Government currently has an agreement with Pfizer for 40 million doses. But while more than a million doses have arrived on our shores and around 130,000 doses are currently being delivered each week, the majority are not expected to arrive until the final quarter of 2021.
Prime Minister Scott Morrison says he hopes the majority of people under 50 will be immunised in the final three months of the year, with the assistance of mass vaccination hubs.
‘There’s a lot of work to be done given that would be effectively, if we wished, a 12-week sprint,’ he said.
‘To be able to do that safely and effectively ... there’d need to be plenty of planning to achieve that.’
Dr Willett says it is with younger cohorts that mass vaccination hubs will become a ‘necessary’ part of the rollout.
‘But certainly for the over-75s, it is much better getting vaccinated at their local GP and I would suggest that the over-65s would likewise … because by that age, most people will have some medical problems,’ he said.
‘But at the moment there’s really three parts: there’s the vaccine availability, the vaccine hesitancy and the manpower. Now, the issue is really with the first two.
‘Moving to mass vaccination clinics will actually worsen the vaccination hesitancy, so the answer is to improve the first two: the supply of vaccines to general practices who we can deal with the hesitancy.’
While Dr Haikerwal says mass vaccination is a positive move, he is concerned it may lead to fewer patients receiving both their vaccinations at the same clinic, resulting in practices missing out on the practice inventive payment (PIP).
‘We absolutely support the state on what they’re doing, and in fact, many of our members will probably end up working in those as well, which will be good. So I don’t think we should be scared of it. But we should on an equal footing,’ he said.
‘At the moment the payment system for general practice is a payment for one jab, a second payment for the second jab, and then when you’ve done both there’s a PIP.
‘With mass vaccination, it means most people won’t actually go to the same place for both jabs. So a patient’s rebates for their care will drop by $10. They’ve got to rejig that to make it $5 on each of the jabs.
‘It’s actually the difference between breaking even or making the loss.’
Log in below to join the conversation.
AstraZeneca COVID-19 vaccine rollout
newsGP weekly poll
Within general practice, do you think there are barriers to providing flu vaccinations? If so, what are they?