Feature
Medicare: How did we get here?
Ahead of the Federal Budget, a GP of nearly 50 years has shared his story of Medicare – one he says is ‘full of naivety, misconceptions, deceptions’.
 By the time Medicare began, around 92% of the Australian population had signed up.
By the time Medicare began, around 92% of the Australian population had signed up.
When Medicare was first introduced forty years ago, following a few failed launches of universal healthcare in Australia, doctors rejoiced that they would finally get reimbursed for consults that had previously been unpaid or left to bad debt.
But if GP and RACGP History Committee Deputy Chair Associate Professor Christopher Hogan had listened to the ‘prophetic’ warnings about Medicare in the beginning, he may have been more prepared for what was to come.
As the final touches are added to the 2024–25 Federal Budget, newsGP has taken a look back at Medicare, its history, and where it is headed.
The year was 1975, Associate Professor Hogan had just graduated, and Prime Minister Gough Whitlam’s government had just got its universal health insurance Medibank off the ground following a double dissolution election and a high court challenge.
The Australian Medical Association had set up a ‘Freedom Fund’ to push back against the ‘interference by governments in the relationship between doctor and patient’ in 1973.
To say there had been some strong pushback would be an understatement.
It was the first scheme where the Federal Government collected taxation to pay out as medical service rebates.
Prior to this, it was not uncommon for Australians to go bankrupt when in dire medical straits – with a scattered private health system and no safety net for those who could not afford it.
When Whitlam’s Labor Government was dismissed that same year, promises made to maintain Medibank led to several reincarnations of the program during the leadership of Liberal Prime Minister Malcolm Fraser.
Eventually the idea was scrapped all together, until 1984 when it was revived by Bob Hawke’s Labor Government and rebranded Medicare.
In 1987, Prime Minister John Howard said Medicare was ‘one of the great failures of the Hawke Government’ and urged it to ‘take a knife’ to the ‘expensive, failed Medicare system’.
Associate Professor Hogan said the story of universal healthcare in Australia has been long and obtuse.
‘It’s full of naivety, misconceptions, deceptions, malice and betrayal,’ he said.
‘When I graduated in 1975, I would have expected over my lifetime to have had the same income as other non-GP specialists would have had.
‘But that’s been progressively eroded over the years.’
It is no secret that Medicare has been pushing GPs to their limit for some time.
With the last decade bringing budget cuts, including a six-year rebate freeze, it is also no surprise that Federal Health and Aged Care Minister Mark Butler said in 2023 that Medicare was in its ‘worst shape in 40 years’.
This response came in light of some hopeful news from the Albanese Government, with a $2.2 billion Medicare investment announced last year.
Officially celebrating Medicare’s 40th birthday in January, RACGP President Dr Nicole Higgins said the initiative, just like general practice, is the foundation of Australia’s health system.
By the time Medicare began, more than 14 million Australians, around 92% of the population, had signed up.
Since then, Medicare has paid over $488 billion in benefits and in its first financial year, it cut the cost of healthcare so dramatically that inflation fell from 6.5% to 3.9%.
So, what went wrong for GPs at the start?
Associate Professor Hogan said the first driver that set GPs on a downward trajectory was their own fierce independence and lack of collective organisation right from the beginning.
‘The [RACGP] was designed around the 50s, it was designed to bring GPs together,’ he said.
‘Really, there was a lot of fragmentation.
‘The academic part of general practice was in its infancy and so [the Government] really didn’t understand what GPs did.’
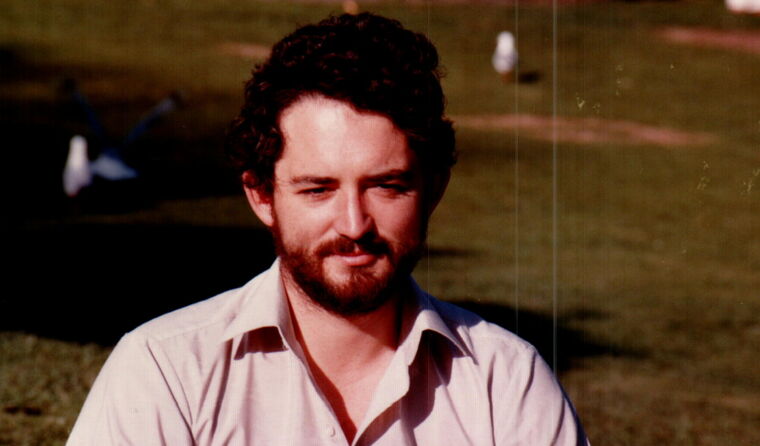
Associate Professor Chris Hogan said he was ‘warned’ about Medicare in the 1980s.
But once the ball really got rolling on Medicare, Associate Professor Hogan said general practice was predominately on-board despite early protestations.
‘It was amazing,’ he said.
‘Prior to that we had about 20% of our patients that either we didn’t charge or they wouldn’t pay.
‘All of a sudden, you were being paid something for that and all of a sudden bad debts weren’t that massive.’
Associate Professor Hogan said he could now see why people in the 80s were wary of the scheme due to ghosts of governments past.
‘What we were warned about Medicare was rather prophetic,’ he said.
‘They said what would happen is that Medicare would come in, everybody would sign up to it, and then that would protect the sector.
‘But then they would, because it was the mark of most of the governments that have had universal health insurance, progressively reduce the payments.
‘We were told that if we took the government shilling, we were dooming ourselves to unemployment.’
Despite being used as a political football through the years, particularly with the 2016 Mediscare campaign, Associate Professor Hogan said the concept has never been adequately funded by any side of the political spectrum – especially when it comes to general practice.
‘The whole political response to general practice has been one of obfuscation, of blurring the boundaries and not being totally open and frank as to what they’re trying to do,’ he said.
‘From the start, Medicare rebates stopped keeping track with the consumer price index (CPI).
‘The value that we were getting back from Medicare didn’t improve.’
Associate Professor Hogan said taxation levies had never ‘adequately renumerated the costs of Medicare’.
‘CPI is a measure of general inflation but in medicine, the inflation rate is two to three times that of CPI,’ he said.
Analysis by the Australian Medical Association in 2022 showed that Medicare has failed to keep up with the real-life costs of operating a medical practice.
‘It gets to a mind-blowing level of deception or misdirection,’ said Associate Professor Hogan.
The Federal Government’s latest budget is set to be revealed on Tuesday morning, with a projected health spend of $8.5 billion for 2024-25.
But concerns have already been raised over whether that money is headed in the right direction.
As for the future of Medicare, Associate Professor Hogan said his colleagues had summed his prognosis up perfectly when it comes to the perspective of general practice.
‘[Governments do not] understand the complex and significant role of general practice and devalues that significantly,’ he said.
‘GPs are in a situation where we’re going to have to charge private fees. Because if we don’t, we simply won’t be able to survive.’
Log in below to join the conversation.
budget Federal Budget general practice Medicare universal healthcare
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?